Does SPN really matter?
February 23, 2022
Glycerophosphate Compatibility
February 27, 2022immunity as a pivotal role in response to injury in the critically ill patient, immune modulating strategies in the critically ill include:
- Pharmacological modulation.
- Extracorporeal removal of inflammatory mediators.
However, little evidence supports the efficacy of immune modulation in critically ill patients.
Normal functioning of the immune system is crucial to the health.
The immune response to injury is highly dynamic and has both pro and anti-inflammatory components. The aim is keeping dynamic regulation within the normal range, as shown in green in the illustration below. Although immune modulation is aimed in many clinical trials, there are no markers allowing conclusions to be drawn on the modulation of immunity.

The pathophysiology of the critically ill patients.
Our immunity has two components: innate immunity and adaptive immunity. When a patient receives a trauma, as an example: surgery, infection, burn or whatever, the usual response is Systemic Inflammatory Response or SIRS response, and this is beneficial. If SIRS response is exaggerated, it may cause early multi system organ failure and in fulminant death of the patient.
On the other hand, we have another system operating in the opposite way of SIRS. This is CARS; Compensatory and Inflammatory Response Syndrome, and there should be a balance between SIRS and CARS.
If CARS is exaggerated, it will cause progressive immunosuppression and may cause indolent death of the patient.
If the management of the patient was good, the patient will recover and return to homeostasis. This is an uncomplicated outcome.
But if SIRS is exaggerated, or CARS is exaggerated, then the patient will have a complicated outcome. And this may cause the death of a patient.
While some patients with severe inflammation may benefit from anti-inflammatory therapies, it’s likely that these therapies should be carefully targeted.
Conversely, many patients with sepsis may benefit from immune stimulation to reverse immuno-paralysis. Unfortunately, they do not have immune markers, and we don’t know the immune status of our patients in this scenario. In summary, immune modulation trials may be dangerous.

Conclusion regarding pathophysiology
What we conclude from pathophysiology studies is inflammation is generally a beneficial response to trauma or illness required to trigger an immune response.
On the other hand, immune modulation, including lipids, has potential to be this disadvantageous.
Expectations from parenteral lipids
What are our expectations of parenteral lipids?
- To meet calorie intake
- To reduce the osmolarity.
- To reduce the risk of hyperglycemia.
- To enhance the bioavailability of fat-soluble vitamins.
- Or to provide essential fatty acids.
I think we all agree that these are our expectations from parenteral lipids.
What about immune modulations?
After infusion of soybean-oil-based lipid emulsions, a predominantly pro-inflammatory pattern is observed.
RANDOMIZED CONTROL TRIAL

This is a clinical study performed in 42 volunteers. This is a randomized control trial. And these volunteers received either soybean oil or fish oil-based lipid emulsions for normal saline.
Then these volunteers inhaled pre-defined doses of lipopolysaccharide and bronchoalveolar lavage (BAL) was performed 8 or 24 hours later to study TNF-a levels. The authors showed that leukocytes exhibited increased pro inflammatory features after infusion of soybean emulsion. On the other hand, fish oil exhibited anti-inflammatory pattern.
Olive-Oil Maintains Protective Immunity

This study assessed the impact of olive oil and soybean oil on lymphocyte proliferation, lymphocytes were collected from healthy volunteers and lymphocyte proliferation was assessed with thymidine incorporation.
In this immature study, at those dependent inhibitions of thymidine incorporation was observed with soybean oil, whereas olive oil has no inhibitory effect.
Summary
In summary, soybean oil is the most suppressive and all the always neutral.
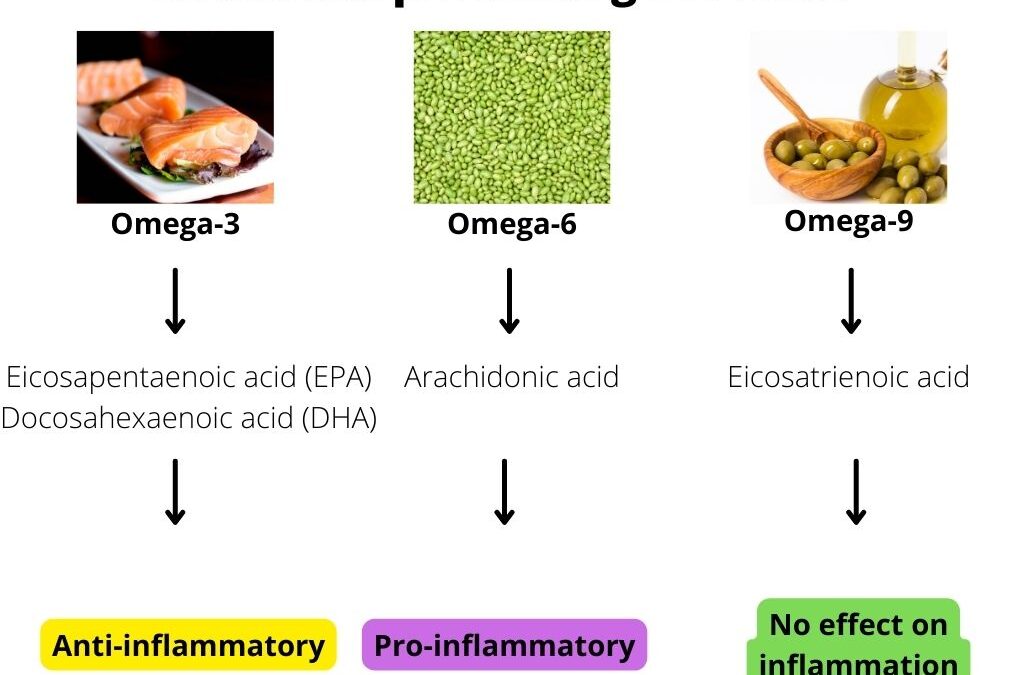
Why does fatty acid have different effects on immunity?
The answer is because of their metabolites.

Let’s start with fish oil Omega three polyunsaturated fatty acids. These fatty acids are converted to Eicosapentaenoic acid (EPA) and Docosahexaenoic acid (DHA) which has anti-inflammatory properties.
On the other hand, Omega six polyunsaturated fatty acids for soybean oil is converted to Arachidonic acid metabolites, which have pro-inflammatory effects and finally, Omega-9 polyunsaturated fatty acids or olive oil is converted to Eicosatrienoic acid and fortunately it has no effect on immunity and inflammation.
Conclusion
Modulating immunity by parenteral lipids has the potential to be unfavorable depending on the condition of the patient and immunological neutrality and preserving immune function are advantages of olive oil based intravenous lipids emulsions.
References
- Cutuli SL, Carelli S, Grieco DL, De Pascale G. Immune Modulation in Critically Ill Septic Patients. Medicina (Kaunas). 2021 May 31;57(6):552. doi: 10.3390/medicina57060552. PMID: 34072649; PMCID: PMC8226671.
- Calder PC, Waitzberg DL, Klek S, Martindale RG. Lipids in Parenteral Nutrition: Biological Aspects. JPEN J Parenter Enteral Nutr. 2020 Feb;44 Suppl 1:S21-S27. doi: 10.1002/jpen.1756. PMID: 32049394.
- Granato D, Blum S, Rössle C, Le Boucher J, Malnoë A, Dutot G. Effects of parenteral lipid emulsions with different fatty acid composition on immune cell functions in vitro. JPEN J Parenter Enteral Nutr. 2000 Mar-Apr;24(2):113-8. doi: 10.1177/0148607100024002113. PMID: 10772192.
- Hecker M, Mayer K. Intravenous lipids in adult intensive care unit patients. World Rev Nutr Diet. 2015;112:120-6. doi: 10.1159/000365667. Epub 2014 Nov 24. PMID: 25471808.
- Albers R, Bourdet-Sicard R, Braun D, Calder PC, Herz U, Lambert C, Lenoir-Wijnkoop I, Méheust A, Ouwehand A, Phothirath P, Sako T, Salminen S, Siemensma A, van Loveren H, Sack U. Monitoring immune modulation by nutrition in the general population: identifying and substantiating effects on human health. Br J Nutr. 2013 Aug;110 Suppl 2:S1-30. doi: 10.1017/S0007114513001505. PMID: 23902657.