What is Mercaptopurine and How Does it Work?
Mercaptopurine: A Cornerstone in Treating Childhood Acute Lymphoblastic Leukemia
Mercaptopurine, often referred to by its chemical name 6-mercaptopurine or simply 6-MP, stands as a pivotal medication in the oncology sphere, particularly within the context of treating childhood Acute Lymphoblastic Leukemia (ALL). This powerful chemotherapeutic agent has significantly advanced the management of pediatric ALL, transforming what was once a uniformly fatal disease into one with high rates of long-term survival. Through the exploration of its mechanism, application, and the tailored approach afforded by pharmacogenomics, mercaptopurine’s role in childhood ALL treatment is both dynamic and indispensable.
What is Mercaptopurine and How Does it Work?
Definition and history of mercaptopurine
Mercaptopurine, a cornerstone in the treatment of childhood acute lymphoblastic leukemia (ALL), possesses a storied history in pediatric oncology. Synthesized in the mid-20th century, this thiopurine analogue quickly became a mainstay in chemotherapy protocols designed to combat pediatric acute lymphoblastic leukemia. As a potent antimetabolite, mercaptopurine disrupts DNA and RNA synthesis, effectively halting the proliferation of leukemic cells within the bone marrow of affected children. Its discovery marked a pivotal moment in the oncology group’s ongoing battle against childhood cancers, facilitating advancements in maintenance therapy and improving survival rates dramatically.
Expanding upon its foundational role, mercaptopurine’s integration into pediatric treatment regimens underscored a significant leap forward in the pediatric oncology field, particularly for acute lymphocytic leukemia. This leap wasn’t just technical; it was transformative, ensuring that children with acute lymphoblastic leukemia could look towards a future beyond their diagnosis. As the backbone of maintenance treatment, mercaptopurine helped shape an oncological landscape where childhood acute lymphoblastic leukaemia transitioned from a fatal diagnosis to one of manageable condition, thereby ushering in an era of hope and progression in pediatric patient care.
Mechanism of action: Incorporation into DNA and RNA
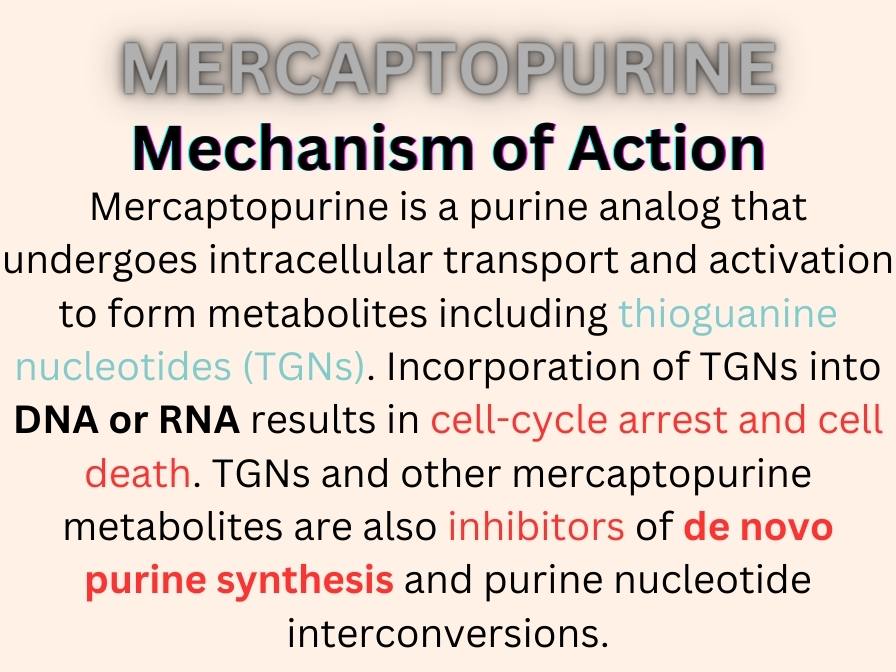
The efficacy of mercaptopurine in the treatment of acute lymphoblastic leukemia (ALL) in children hinges on its sophisticated mechanism of action. By mimicking the structure of natural nucleotides, mercaptopurine deceives the cellular machinery into incorporating itself into the DNA and RNA of rapidly dividing cells, including malignant leukocytes.
This incorporation leads to a cascade of events that ultimately results in the inhibition of nucleotide biosynthesis, a critical pathway for DNA replication and repair. The disruption of this pathway is particularly detrimental to leukemia cells, thereby slowing disease progression and providing a therapeutic edge in the treatment of childhood ALL.
Through the blockage of purine synthesis, mercaptopurine precisely targets the Achilles heel of leukemic cells — their unbridled proliferation. This targeted approach not only disrupts the leukemic cells’ lifecycle but also spares healthy cells, minimizing collateral damage.
This selective toxicity is a hallmark of effective chemotherapy regimens, making mercaptopurine a critical weapon in the pediatric oncologist’s arsenal against childhood acute lymphoblastic leukaemia.
| Parameter | (Adults) | Pediatric |
|---|---|---|
| Peak Concentration | 93 ng/mL (range: 40-204 ng/mL) | – |
| Time to Peak | 0.75 hours (range: 0.33-2.5 hours) | 1-3 hours |
| Area Under the Curve | 137 hr x ng/mL (range: 77-268 hr x ng/mL) | AUC(1 to 5 hours): 56 micromolar x min (range: 23-65 micromolar x min) |
Role as an antimetabolite and thiopurine
Alongside its incorporation into the DNA and RNA of leukemia cells, its role in inhibiting the synthesis of thioguanine nucleotides further augments its mechanism of action, showcasing the multi-faceted approach mercaptopurine employs to combat ALL.
By not only halting replication but also imposing genetic instability upon leukemia cells, mercaptopurine ensures a multi-pronged attack against the disease, spotlighting the sophisticated chemical warfare that defines modern chemotherapy.
The Importance of Mercaptopurine in Treating Childhood ALL
Mercaptopurine as a cornerstone of ALL maintenance therapy
Within the structured phases of ALL treatment, maintenance therapy assumes a crucial role, aiming to sustain remission and forestall relapse. Mercaptopurine’s inclusion in maintenance regimens reflects its proven efficacy in achieving these goals, anchoring a treatment phase that is pivotal for long-term survival.
The drug’s ability to undermine leukemic proliferation while sparing the normal hematopoietic function exemplifies its ideal suitability for prolonged administration during this treatment phase.
Improved survival rates and reduced risk of relapse
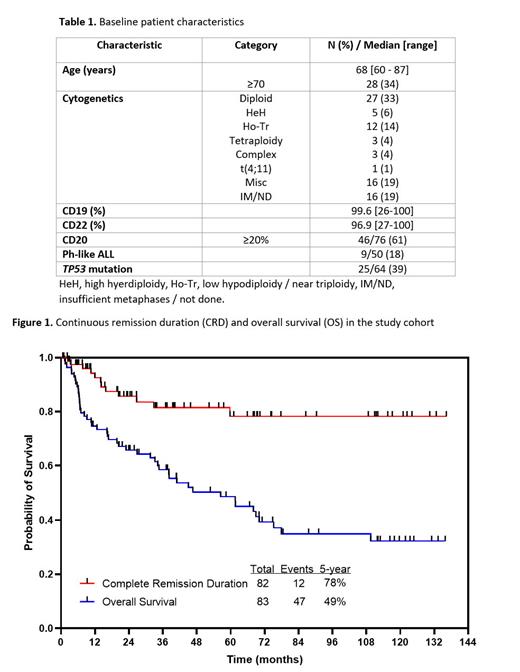
The introduction of mercaptopurine into the treatment landscape for childhood acute lymphoblastic leukemia (ALL) has been a game-changer, significantly bolstering survival rates and diminishing the threat of disease relapse. link
The strategic deployment of mercaptopurine in therapy regimens leverages its biochemical mechanisms to maintain a therapeutic assault on leukemia cells, thereby securing the strides made during earlier phases of treatment. This sustained offensive is crucial in extending the disease-free interval for pediatric patients, effectively reducing the incidence of relapse and cementing mercaptopurine’s role in promoting long-term survival.
The adopted protocol, the stratification profile and outcome of children with ALL, treated with modified UKALL 97(99) and UKALL 2003 in the authors’ institution from 2006 to 2014 are reported. Via
Comparative studies and clinical trials have consistently highlighted the remarkable impact of mercaptopurine on survival outcomes in children with acute lymphoblastic leukemia. By meticulously impairing leukemic cell proliferation, mercaptopurine not only extends life expectancy but also enhances the quality of life for survivors, minimizing the psychosocial and physical burdens of a potential relapse.
More references here, here and here.
Psychosocial Burdens:
Feeling scared and sad: Kids and their families might feel more worried, sad, and scared than before.
Family stress: The family might face more stress, with parents and siblings feeling extra pressure and possibly less attention to everyone’s needs.
Feeling alone: Kids might not see their friends much because they’re often in the hospital or can’t go to school, making them feel lonely.
Missing school: Kids might miss a lot of school because they’re getting treatment, which can make keeping up with studies hard.
Money worries for the family: The cost of treatment can make families worry about how to pay for everything.
Physical Burdens:
Tougher treatment: If acute lymphocytic leukemia comes back, the treatment might be stronger and harder on the body, sometimes necessitating transplantation.
More side effects: Side effects like feeling sick, tired, losing hair, and getting infections can be worse with stronger treatment.
Getting sick easier: The treatment can make it easier for kids to catch infections and colds because their immune system is weaker.
Growth problems: Treatment can affect how kids grow and develop.
Feeling pain: The treatments and tests can be painful and uncomfortable.
Comparison with other chemotherapy agents
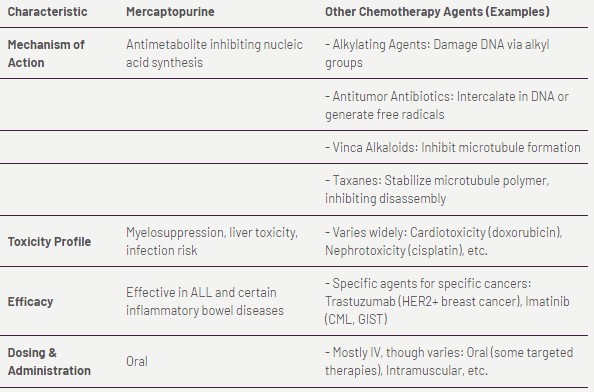
In the realm of pediatric oncology, mercaptopurine stands out for its distinguished role in treating childhood acute lymphoblastic leukemia (ALL). When juxtaposed with other chemotherapy agents, mercaptopurine’s unique mechanism of action and its pivotal role in maintenance therapy underscore its singular importance.
While other drugs may target different aspects of cancer cell growth or harness alternative biochemical pathways, mercaptopurine’s ability to integrate into DNA and RNA synthesis presents a critical lever in the maintenance phase of ALL treatment, a phase geared towards sustaining remission and mitigating relapse risks.
Its combination with drugs like methotrexate amplifies the therapeutic impact, demonstrating a concerted effort to eradicate leukemic cells comprehensively.
Dosage and Administration of Mercaptopurine in Pediatric ALL
Standard dosing regimens for children
The administration of mercaptopurine in pediatric patients diagnosed with acute lymphoblastic leukemia (ALL) follows carefully calibrated dosing regimens, meticulously designed to optimize therapeutic outcomes while mitigating potential toxicities. These regimens consider a myriad of factors, including the patient’s weight, stage of treatment, and individual response to therapy, ensuring that each child receives the most effective dose tailored to their specific needs.
The precision of dosing is crucial, as it balances the drug’s potent anti-leukemic effects against the risk of adverse reactions, marking a delicate yet critical aspect of pediatric ALL management.
Acute lymphoid leukemia, Maintenance therapy, as part of combination chemotherapy
Mercaptopurine Desensitization Protocol
| Day | Total Daily Dose (mg) |
| 1 | 0.05 |
| 2 | 0.10 |
| 3 | 0.15 |
| 4 | 0.5 |
| 5 | 1 |
| 6 | 2.5 |
| 7 | 5 |
| 8 | 10 |
| 9 | 25 |
| 10 | 25 |
| 11 | 25 |
| 12 | 25 |
| 13 | 50 |
| *Capsules containing 0.05 mg, 0.5 mg, and 5 mg were prepared for the desensitization protocol | |
Factors influencing dosage adjustments
Dosage adjustments of mercaptopurine in pediatric ALL treatment are influenced by a constellation of factors, each pivotal in tailoring therapy to the nuanced needs of the individual patient.
Testing for thiopurine S-methyltransferase (TPMT) activity, for instance, offers invaluable insights into a patient’s ability to metabolize mercaptopurine, guiding dose optimization to avoid toxicity while maintaining anti-leukemic efficacy.
Dosage in Renal Failure
Consider initiating at the low end of the dosing range in renally impaired patients, or increase the dosing interval to 36 to 48 hours in patients with CrCl less than 50 mL/min. Ref.
Dosage in Hepatic Insufficiency
Consider dosage reduction or initiate at the low end of the dosing range and monitor closely for toxicity.
Dosage in Other Disease States
A) Concomitant Use
1) With allopurinol: Reduce mercaptopurine to one-third to one-quarter of usual dose. Ref.
2) With aminosalicylate derivatives: Use the lowest possible dose of each drug. Ref.
B) Myelosuppression
Excessive hematological toxicity: Maintain absolute neutrophil count at a desirable level by reducing the dose. Ref.
C) Thiopurine Methyltransferase (TPMT) and/or Nucleotide Diphosphatase (NUDT15) Mutations
1) TPMT genotype is strongly linked to TPMT phenotype, therefore these recommendations apply regardless of the method used to assess TPMT status. NUDT15 phenotypes are based on the most common allele diplotypes:
| Phenotype | Dosage Adjustment |
| NUDT15 normal metabolizer (eg, *1/*1) | No adjustment needed to initial dose. Normal starting doses vary by race/ethnicity and treatment regimens. |
| Adjust dosage of mercaptopurine or other myelosuppressive agents as needed, without emphasis on mercaptopurine allowing at least 2 weeks to reach steady-state after each dose adjustment. | |
| NUDT15 intermediate metabolizer (eg, *1/*2, *1/*3) or possible intermediate metabolizer (eg, *2/*5, *3/*6) | Normal starting doses vary by race/ethnicity and treatment regimens. |
| If normal starting dose is 75 mg/m(2)/day or greater, or 1.5 mg/kg/day or greater, initiate with 30% to 80% of the normal dose (eg, start at 25 to 60 mg/m(2)/day or 0.45 to 1.2 mg/kg/day), as recommended in oncology group study protocols. Adjust dose as needed based on degree of myelosuppression, allowing at least 2 to 4 weeks to reach steady-state after each adjustment. If myelosuppression occurs, reduce mercaptopurine dosage over other agents. | |
| If normal starting dose is less than 75 mg/m(2)/day, or less than 1.5 mg/kg/day, dosage reduction is not recommended. | |
| NUDT15 poor metabolizer (eg, *2/*2, *2/*3, *3/*3) | In patients with malignancy, initiate with a reduced dose of 10 mg/m(2)/day. Adjust dose as needed based on degree of myelosuppression, allowing at least 4 to 6 weeks to reach steady-state after each adjustment. If myelosuppression occurs, reduce mercaptopurine dosage over other agents. |
| In patients with non-malignant conditions, consider alternative non-thiopurine immunosuppressive therapy. | |
| TPMT normal metabolizer (eg, *1/*1) | Normal starting doses vary by race/ethnicity and treatment regimens. |
| Initiate with normal starting dose and adjust dose as needed based on degree of myelosuppression, allowing at least 2 weeks to reach steady-state after each adjustment. | |
| TPMT intermediate metabolizer (eg, *1/*2, *1/*3A, *1/*3B, *1/*3C, *1/*4) or possible intermediate metabolizer (eg, *2/*8, *3A/*7) | Normal starting doses vary by race/ethnicity and treatment regimens. |
| If normal starting dose is 75 mg/m(2)/day or greater, or 1.5 mg/kg/day or greater, initiate with 30% to 80% of the normal dose (eg, start at 25 to 60 mg/m(2)/day or 0.45 to 1.2 mg/kg/day). Adjust dose as needed based on degree of myelosuppression, allowing at least 2 to 4 weeks to reach steady-state after each adjustment. If myelosuppression occurs, reduce mercaptopurine dosage over other agents. | |
| If normal starting dose is less than 75 mg/m(2)/day, or less than 1.5 mg/kg/day, dosage reduction is not recommended. | |
| TPMT poor metabolizer (eg, *3A/*3A, *2/*3A, *3A/*3C, *3C/*4, *2/*3C, *3A/*4) | In patients with malignancy, initiate with a markedly reduced daily dose; 10-fold reduction in dose and reduce frequency to 3 times a week instead of daily (eg, 10 mg/m(2)/day administered 3 days/week). Adjust dose as needed based on degree of myelosuppression, allowing at least 4 to 6 weeks to reach steady-state after each adjustment. If myelosuppression occurs, reduce mercaptopurine dosage over other agents. |
| In patients with non-malignant conditions, consider alternative non-thiopurine immunosuppressive therapy. | |
| TPMT normal metabolizer (eg, *1/*1) Plus NUDT15 normal metabolizer (eg, *1/*1) | No adjustment needed |
| TPMT normal metabolizer (eg, *1/*1) Plus NUDT15 intermediate metabolizer (eg, *1/*2, *1/*3) | Consider dosage reduction. Normal starting doses vary by race/ethnicity and treatment regimens. |
| If normal starting dose is 75 mg/m(2)/day or greater, or 1.5 mg/kg/day or greater, initiate with 30% to 80% of the normal dose (eg, start at 25 to 60 mg/m(2)/day or 0.45 to 1.2 mg/kg/day). Adjust dose as needed based on degree of myelosuppression, allowing at least 2 to 4 weeks to reach steady-state after each adjustment. If myelosuppression occurs, reduce mercaptopurine dosage over other agents. | |
| If normal starting dose is less than 75 mg/m(2)/day, or less than 1.5 mg/kg/day, dosage reduction is not recommended. | |
| TPMT normal metabolizer (eg, *1/*1) Plus NUDT15 poor metabolizer (eg, *2/*2, *2/*3, *3/*3) | Dosage reductions recommended. Normal starting doses vary by race/ethnicity and treatment regimens. |
| In patients with malignancy, initiate with a reduced dose of 10 mg/m(2)/day. Adjust dose as needed based on degree of myelosuppression, allowing at least 4 to 6 weeks to reach steady-state after each adjustment. If myelosuppression occurs, reduce mercaptopurine dosage over other agents. | |
| In patients with non-malignant conditions, consider alternative non-thiopurine immunosuppressive therapy. | |
| TPMT intermediate metabolizer (eg, *1/*2, *1/*3A, *1/*3B, *1/*3C, *1/*4) Plus NUDT15 normal metabolizer (eg, *1/*1) | Consider dose reduction. Normal starting doses vary by race/ethnicity and treatment regimens. |
| If normal starting dose is 75 mg/m(2)/day or greater, or 1.5 mg/kg/day or greater, initiate with 30% to 80% of the normal dose (eg, start at 25 to 60 mg/m(2)/day or 0.45 to 1.2 mg/kg/day). Adjust dose as needed based on degree of myelosuppression, allowing at least 2 to 4 weeks to reach steady-state after each adjustment. If myelosuppression occurs, reduce mercaptopurine dosage over other agents. | |
| If normal starting dose is less than 75 mg/m(2)/day, or less than 1.5 mg/kg/day, dosage reduction is not recommended. | |
| TPMT intermediate metabolizer (eg, *1/*2, *1/*3A, *1/*3B, *1/*3C, *1/*4) Plus NUDT15 intermediate metabolizer (eg, *1/*2, *1/*3) | Dosage reductions recommended. Normal starting doses vary by race/ethnicity and treatment regimens. |
| If normal starting dose is 75 mg/m(2)/day or greater, or 1.5 mg/kg/day or greater, initiate with 30% to 80% of the normal dose (eg, start at 25 to 60 mg/m(2)/day or 0.45 to 1.2 mg/kg/day). Adjust dose as needed based on degree of myelosuppression, allowing at least 2 to 4 weeks to reach steady-state after each adjustment. If myelosuppression occurs, reduce mercaptopurine dosage over other agents. | |
| If normal starting dose is less than 75 mg/m(2)/day, or less than 1.5 mg/kg/day, dosage reduction is not recommended. | |
| TPMT intermediate metabolizer (eg, *1/*2, *1/*3A, *1/*3B, *1/*3C, *1/*4) Plus NUDT15 poor metabolizer (eg, *2/*2, *2/*3, *3/*3) | Dosage reductions recommended. Normal starting doses vary by race/ethnicity and treatment regimens. |
| In patients with malignancy, initiate with a reduced dose of 10 mg/m(2)/day. Adjust dose as needed based on degree of myelosuppression, allowing at least 4 to 6 weeks to reach steady-state after each adjustment. If myelosuppression occurs, reduce mercaptopurine dosage over other agents. | |
| In patients with non-malignant conditions, consider alternative non-thiopurine immunosuppressive therapy. | |
| TPMT poor metabolizer (eg, *3A/*3A, *2/*3A, *3A/*3C, *3C/*4, *2/*3C, *3A/*4) Plus NUDT15 normal metabolizer (eg, *1/*1), NUDT15 intermediate metabolizer (eg, *1/*2, *1/*3), or NUDT15 poor metabolizer (eg, *2/*2, *2/*3, *3/*3) | Dosage reductions recommended. Normal starting doses vary by race/ethnicity and treatment regimens. |
| In patients with malignancy, initiate with a markedly reduced daily dose; 10-fold reduction in dose and reduce frequency to 3 times a week instead of daily (eg, 10 mg/m(2)/day administered 3 days/week). Adjust dose as needed based on degree of myelosuppression, allowing at least 4 to 6 weeks to reach steady-state after each adjustment. If myelosuppression occurs, reduce mercaptopurine dosage over other agents. | |
| In patients with non-malignant conditions, consider alternative non-thiopurine immunosuppressive therapy. |
2) Heterozygous thiopurine S-methyltransferase (TPMT) or nucleotide diphosphatase (NUDT15) enzyme deficiency: Reduce dosage based on tolerability; most patients tolerate usual doses; heterozygous for both TPMT and NUDT15 may require more substantial dosage reductions. Ref / Ref.
3) Homozygous TPMT or NUDT15 enzyme deficiency: Reduce initial dosage; patients typically require 10% or less of the usual dosage. Ref / Ref.
Importance of adherence to prescribed treatment
Adherence to the prescribed mercaptopurine regimen is paramount in the successful treatment of pediatric acute lymphoblastic leukemia (ALL). The drug’s role in maintaining long-term remission hinges on consistent administration, as lapses can precipitate a resurgence of leukemic activity and potentially compromise survival outcomes. The importance of adherence is underscored by the delicate balance between achieving therapeutic efficacy and avoiding undue toxicities, a balance that necessitates unwavering commitment to prescribed treatment schedules.
Maintenance of Remission: Adherence to mercaptopurine therapy is essential for maintaining remission in pediatric ALL. Mercaptopurine is a cornerstone of maintenance therapy in pediatric ALL regimens, and consistent adherence to the prescribed treatment schedule is critical for preventing disease relapse during this phase of treatment.
Reduction of Relapse Risk: Mercaptopurine plays a pivotal role in reducing the risk of relapse in pediatric ALL. Adherence to mercaptopurine therapy as part of the maintenance regimen has been associated with improved long-term outcomes, including a lower risk of disease recurrence.
Optimization of Chemotherapy Efficacy: Adherence to mercaptopurine treatment contributes to the overall efficacy of chemotherapy for acute lymphoblastic leukemia in pediatric ALL. Consistent administration of mercaptopurine as prescribed by healthcare providers ensures that the drug can exert its intended anti-leukemic effects, thereby contributing to the success of the comprehensive treatment protocol.
Prevention of Drug Resistance: Non-adherence to mercaptopurine therapy can potentially lead to the development of drug resistance in leukemia cells. By adhering to the prescribed treatment regimen, pediatric ALL patients can help minimize the risk of resistance, thereby preserving the effectiveness of mercaptopurine and other chemotherapy agents used in their treatment.
Long-Term Survival and Quality of Life: Adherence to mercaptopurine therapy has been linked to improved long-term survival rates and enhanced quality of life in pediatric ALL survivors. By following the prescribed treatment plan, patients can maximize their chances of achieving durable remission and long-term disease-free survival.
Potential Side Effects and Toxicities of Mercaptopurine
Common adverse effects: Myelosuppression, hepatotoxicity, and pancreatitis
Mercaptopurine, while a cornerstone in the treatment of childhood acute lymphoblastic leukemia (ALL), carries with it a spectrum of potential side effects and toxicities that necessitate vigilant monitoring.
Among the most clinically significant adverse effects are myelosuppression, hepatotoxicity, and pancreatitis, each presenting unique challenges in the context of pediatric care.
Myelosuppression, characterized by the decrease in the production of blood cells, exposes patients to risks of infection, anemia, and bleeding, underscoring the need for regular blood count monitoring. Hepatotoxicity manifests through elevated liver enzymes, signaling potential liver damage, while pancreatitis, though less common, constitutes a severe and potentially life-threatening condition.
The management of these toxicities involves a multidisciplinary approach, emphasizing the importance of early detection and intervention. Regular liver function tests and pancreatic enzyme assays are part of the comprehensive surveillance strategy employed to identify hepatotoxicity and pancreatitis at their nascent stages.
Similarly, the close monitoring of complete blood counts facilitates the timely identification and management of myelosuppression, allowing for dose adjustments or temporary cessation of therapy to mitigate risks. This proactive approach not only minimizes the impact of adverse effects on quality of life but also ensures the continuity of essential treatment for pediatric ALL patients.
| Side Effect | Information |
|---|---|
| Alopecia | Reported as a delayed or late toxicity of mercaptopurine therapy. |
| Erythematous rash | Transient rash occurring after mercaptopurine/methotrexate maintenance therapy, pruritic with papular and/or scaly component, primarily around the mouth, upper chest, dorsal forearms, and hands. Resistant to treatment but clears spontaneously. |
| Hyperpigmentation | Incidence: Less than 5%. |
| Photosensitivity | Reported postmarketing. |
| Rash | Incidence: 5% to 20%. Occurs in acute lymphoblastic leukemia clinical trials. |
| Urticaria | Incidence: Less than 5%. Seen in acute lymphoblastic leukemia clinical trials. |
| Endocrine/Metabolic Effects | – Hyperuricemia: Incidence less than 5% in acute lymphoblastic leukemia clinical trials. – Hypoglycemia: Reported postmarketing. – Hypoglycemia-induced convulsion: Case of nocturnal seizure linked to severe hypoglycemia in a child with acute lymphoblastic leukemia receiving mercaptopurine. Treated with D10W IV bolus. |
| Gastrointestinal Effects | – Diarrhea: Incidence 5% to 20%. Seen in acute lymphoblastic leukemia clinical trials. – Loss of appetite: Incidence 5% to 20%. Seen in acute lymphoblastic leukemia clinical trials. – Nausea: Incidence 5% to 20%. Seen in acute lymphoblastic leukemia clinical trials. – Oral lesion: Resembles thrush, incidence less than 5%. |
| – Pancreatitis: Incidence less than 5%. Onset within days of therapy initiation. Resolves within days post-discontinuation. Recurrence on rechallenge within days. Isolated cases reported in Crohn’s disease or ulcerative colitis patients on mercaptopurine. | |
| – Vomiting: Incidence 5% to 20%. Seen in acute lymphoblastic leukemia clinical trials. | |
| Hematologic Effects | – Autoimmune hemolytic anemia: Reported in an adult case after mercaptopurine treatment for chronic myelomonocytic leukemia. – Myelosuppression: Incidence greater than 20%. Dose-related toxicity characterized by anemia, leukopenia, thrombocytopenia, or combination. Risk increased with enzyme deficiency or coadministration of myelosuppressive agents. |
| Hepatic Effects | – Ascites, Hepatic encephalopathy, Hepatic fibrosis, Hepatic necrosis, Hepatotoxicity, Hyperbilirubinemia, Jaundice, Liver function tests outside reference range, Portal hypertension are complications that can arise from the hepatotoxic effects of treatments like 6MP in acute lymphoblastic leukemia.: Various hepatic issues reported. |
| Immunologic Effects | – Hypersensitivity reaction: Allergic reactions seen in inflammatory bowel disease patients on mercaptopurine. Symptoms include fever, joint pain, back pain, sepsis-like syndrome, and more. – Infectious disease: Incidence less than 5%. – Lymphoproliferative disorder: Reported malignancies due to mercaptopurine therapy. Risk linked to immunosuppression. |
| – Macrophage activation syndrome: Can occur in autoimmune patients on mercaptopurine. Linked to EBV and CMV infections. Treat promptly and discontinue if suspected or confirmed. – T-cell lymphoma, Hepatosplenic: Reported cases primarily in adolescents and young adults being treated for inflammatory bowel disease; most cases were fatal. | |
| Reproductive Effects | – Oligozoospermia: Reported as a delayed toxicity of mercaptopurine therapy. |
| Respiratory Effects | – Pulmonary fibrosis: Reported as a delayed toxicity of mercaptopurine therapy. |
| Other | – Drug-induced hyperpyrexia: Drug fever reported in clinical trials. – Malaise: Incidence 5% to 20%, seen in acute lymphoblastic leukemia clinical trials. – Metastatic malignant neoplasm: Reported malignancies due to mercaptopurine therapy, especially in cases of prolonged immunosuppression. |
| – Serum sickness caused by drug: Case report of serum sickness within weeks of mercaptopurine initiation, resolved upon discontinuation. |
Supportive Care During Mercaptopurine Therapy

Supportive care during Mercaptopurine therapy is critical to ensure that patients not only adhere to the treatment regimen but also maintain an optimal quality of life. One of the primary concerns associated with Mercaptopurine relates to managing nausea, vomiting, and other gastrointestinal symptoms, which are relatively common side effects of this medication.
Moreover, preventing and treating infections constitutes a pivotal aspect of supportive care due to the immunosuppressive nature of Mercaptopurine. This necessitates vigilant monitoring for signs of infection, alongside employing preventive measures such as vaccination and prophylactic antibiotics when indicated, especially in patients undergoing chemotherapy for acute lymphoblastic leukemia. Additionally, maintaining stringent hygiene practices is paramount for minimizing the risk of opportunistic infections.
Lastly, providing psychosocial support for patients and their families is an indispensable component of comprehensive care. The emotional and psychological burdens of chronic illness and ongoing treatment can be substantial. Thus, facilitating access to counseling services, support groups, and educational resources is essential in helping patients and their families navigate the challenges associated with Mercaptopurine therapy. Creating a robust support network, including healthcare providers, mental health professionals, and peer support, can significantly enhance the treatment experience and promote overall wellbeing.
Long-term consequences of mercaptopurine exposure
Long-term exposure to mercaptopurine has been associated with a spectrum of potential side effects and toxicities that must be carefully monitored. Chronic use of mercaptopurine can lead to myelosuppression, where the bone marrow’s ability to produce blood cells is impaired, increasing the risk of infections, anemia, and bleeding. Additionally, there is an elevated risk of developing secondary cancers, such as skin cancers and lymphomas, due to the drug’s mechanism of action on DNA replication and cell division.
On a metabolic level, mercaptopurine can cause abnormalities in liver function tests, signaling potential liver damage or hepatotoxicity, which may progress to more severe conditions with prolonged exposure.
Patients may experience gastrointestinal disturbances, including nausea, vomiting, and pancreatitis, which can significantly impact quality of life.
Mercaptopurine in Combination with Other Agents
Synergistic effects of mercaptopurine and methotrexate
The synergy between these two drugs stems from their complementary mechanisms of action on the purine and pyrimidine biosynthesis pathways, respectively.
While mercaptopurine inhibits the conversion of inosine monophosphate to adenosine monophosphate, thereby affecting the purine salvage pathway, a critical aspect of chemotherapy for acute lymphoblastic leukemia. methotrexate inhibits dihydrofolate reductase, impeding the formation of tetrahydrofolate and, subsequently, thymidylate production. This concerted action results in the amplification of each drug’s effect on DNA synthesis inhibition, effectively leading to enhanced cytotoxicity towards rapidly dividing cells, such as leukemic cells.
Moreover, the use of mercaptopurine in concert with methotrexate can be finely tuned to optimize therapeutic indices, striking a balance between efficacy and toxicity. This has markedly advanced the treatment paradigm for ALL, affording a higher degree of precision in tailoring therapy to individual patient profiles, and ensuring a wider therapeutic window with improved outcomes.
Emerging role of allopurinol in optimizing mercaptopurine therapy
To optimize the therapeutic index of mercaptopurine, recent strategies have emerged that include the adjunct use of allopurinol. Allopurinol, traditionally used in the management of gout and hyperuricemia, acts as a xanthine oxidase inhibitor. By inhibiting xanthine oxidase, allopurinol reduces the conversion of mercaptopurine into its inactive metabolites, thus increasing the availability of mercaptopurine for its therapeutic action. This combination allows for the use of lower doses of mercaptopurine, reducing the risk of myelosuppression and other dose-limiting toxicities, while maintaining, or even enhancing, its antileukemic effects.
Clinically, the mercaptopurine and allopurinol combination offers a promising approach to individualizing therapy, particularly for patients with variations in TPMT activity. This tailored approach not only mitigates the risk of severe toxicity but also ensures that patients receive the most effective dose for their specific metabolic profile. As ongoing research further elucidates the pharmacogenomics of thiopurine metabolism, the role of allopurinol in optimizing mercaptopurine therapy is set to become increasingly significant, heralding a new era in precision medicine for leukemia treatment.
Monitoring Response to Mercaptopurine Treatment
Monitoring response to Mercaptopurine treatment is critical in managing diseases such as acute lymphoblastic leukemia. A key component of this monitoring is assessing minimal residual disease (MRD), which involves detecting the small number of cancer cells that remain after treatment. This assessment helps determine how effectively the Mercaptopurine is working and whether additional or altered treatment is necessary. MRD can provide an early indication of relapse, thereby allowing for timely intervention.
Based on the results of MRD and overall patient response, healthcare providers can make informed decisions about adjusting therapy. This might involve increasing the dose of Mercaptopurine, adding other medications to the regimen, or, in cases of favorable response, possibly reducing treatment intensity to minimize side effects. This tailored approach aims to optimize therapeutic efficacy while managing toxicity.
The role of bone marrow aspirates and biopsies cannot be understated in this process. These procedures are instrumental in evaluating the morphological status of the marrow, aiding in the MRD assessment, and providing valuable information on the treatment’s effectiveness. Through careful analysis of bone marrow samples, clinicians can gain deeper insights into the disease state and make more accurate decisions regarding therapy adjustments.
FAQs about mercaptopurine
Q: What is Mercaptopurine and how does it work in treating childhood acute lymphoblastic leukemia?
A: Mercaptopurine, also known as 6-MP, is a chemotherapy medication used in the treatment of childhood acute lymphoblastic leukemia (ALL). It works by interfering with the synthesis of DNA and RNA, which are necessary for the growth and replication of leukemia cells. By inhibiting these processes, mercaptopurine prevents the proliferation of cancerous cells, effectively contributing to the control and remission of leukemia.
Q: Why is Mercaptopurine often used in conventional chemotherapy protocols for ALL?
A: Mercaptopurine is a cornerstone in conventional chemotherapy protocols for childhood acute lymphoblastic leukemia due to its proven effectiveness and specific action mechanism against leukemia cells. When combined with other drugs, it enhances the overall efficacy of the treatment by targeting different pathways of cancer cell growth and survival, leading to better patient outcomes and higher rates of remission.
Q: What are the common side effects of Mercaptopurine in the treatment of childhood acute lymphoblastic leukemia?
A: Common side effects of Mercaptopurine in treating childhood ALL include myelosuppression (a decrease in the production of blood cells, leading to increased risk of infections, anemia, and bleeding), liver toxicity, nausea, vomiting, and loss of appetite. Regular monitoring and supportive care are important to manage these side effects and ensure the safety and well-being of the patient throughout the treatment course.
Q: Can Mercaptopurine cause tumor lysis syndrome in ALL patients, and how is it managed?
A: Yes, Mercaptopurine can cause tumor lysis syndrome, particularly in the initial phases of treatment, when a large number of leukemia cells are killed rapidly, leading to the release of their contents into the bloodstream. This syndrome can lead to life-threatening electrolyte imbalances and kidney failure. To manage this risk, patients are closely monitored, hydrated, and may receive medications to control uric acid levels, thereby preventing or mitigating the effects of tumor lysis syndrome.
Q: How is the dosage of Mercaptopurine determined for children with acute lymphoblastic leukemia?
A: The dosage of Mercaptopurine for children with ALL is carefully calculated based on the child’s body surface area (BSA) and may be adjusted according to the child’s response to the drug and tolerance of side effects. Regular blood tests are conducted to monitor the effects of the medication on the leukemia cells and the body, allowing for dosage adjustments as needed for efficacy and safety.
Q: What makes Mercaptopurine a preferred choice over newer treatments for some patients?
A: Mercaptopurine remains a preferred choice for some patients due to its long-standing track record of efficacy, affordability, and integrability into multi-drug treatment protocols. While newer treatments are available, mercaptopurine’s specific action on cancer cells, its role in various chemotherapy regimens, and extensive experience with its use make it a fundamental component of therapy for childhood acute lymphoblastic leukemia.
Q: How does resistance to Mercaptopurine develop, and how is it addressed in treatment plans?
A: Resistance to Mercaptopurine can develop through various mechanisms, such as changes in the leukemia cells that affect drug uptake, metabolism, or the repair of DNA damage caused by the drug. To address resistance, clinicians may adjust the dose, add medications that work synergistically with mercaptopurine, or switch to alternative therapies. Ongoing research into resistance mechanisms also informs the development of new strategies to overcome resistance and improve treatment outcomes.
Q: What is the role of genetic testing in the administration of Mercaptopurine for ALL treatment?
A: Genetic testing plays a critical role in the administration of Mercaptopurine for ALL treatment by identifying genetic variations that can affect drug metabolism and response. For instance, variations in the TPMT or NUDT15 genes can increase the risk of toxic side effects from standard doses of mercaptopurine. Identifying patients with these variations allows for dose adjustments to achieve the optimal balance between efficacy and safety, thereby personalizing treatment and improving outcomes.
Q: What is mercaptopurine and its role in treating childhood acute lymphoblastic leukemia?
A: Mercaptopurine is a key medication used in the treatment of childhood acute lymphoblastic leukemia. It is an essential component of chemotherapy regimens aimed at curing this type of cancer.
Q: How does mercaptopurine work in combination with allopurinol?
A: Mercaptopurine is often used in combination with allopurinol to prevent the buildup of toxic byproducts in the body. Allopurinol helps to enhance the effectiveness of mercaptopurine therapy in children with acute lymphoblastic leukemia.
Q: What is the significance of using mercaptopurine in combination with allopurinol in children with acute lymphoblastic leukemia?
A: The combination of mercaptopurine and allopurinol has been shown to improve treatment outcomes in children with acute lymphoblastic leukemia. It helps to minimize side effects and maximize the efficacy of thiopurine-based therapies.
Q: How is mercaptopurine used in acute lymphoblastic leukemia maintenance therapy?
A: Mercaptopurine is a crucial component of maintenance therapy for acute lymphoblastic leukemia. It is administered to prevent the recurrence of cancer cells and maintain remission in patients.
Q: What is the role of pharmacogenomics in optimizing mercaptopurine therapy?
A: Pharmacogenomics helps in tailoring mercaptopurine dosages based on individual genetic factors, a practice that improves outcomes in acute lymphocytic leukemia therapy. This personalized approach enhances treatment outcomes and reduces the risk of adverse reactions to the medication.
Q: What are the key benefits of using mercaptopurine in the treatment of childhood acute lymphoblastic leukemia?
A: Mercaptopurine plays a vital role in increasing the cure rate of acute lymphoblastic leukemia in children. It is an essential component of chemotherapy regimens that have significantly improved the overall survival and event-free survival rates in young patients.
Q: What do studies by oncology groups reveal about the efficacy of mercaptopurine in treating acute lymphoblastic leukemia?
A: Studies conducted by oncology groups demonstrate that mercaptopurine, especially when used in combination with other medications, has a profound impact on the outcomes of acute lymphoblastic leukemia treatment. These studies highlight the importance of mercaptopurine in achieving better results in pediatric oncology.
Patient Education
What is Mercaptopurine used for? Mercaptopurine is used to treat acute lymphoblastic leukemia.
When should Mercaptopurine not be used? Mercaptopurine should not be used if someone had an allergic reaction to it or if they are pregnant.
How should Mercaptopurine be taken? Mercaptopurine can be taken in liquid or tablet form. It is essential to follow the doctor’s instructions closely, and the dose may need to be adjusted. It is often given with other medicines. The oral liquid should be well mixed before use, measured accurately, and stored properly. It is recommended to drink extra fluids.
What should be avoided while taking Mercaptopurine? It is advised to consult a doctor or pharmacist before using other medications, including over-the-counter drugs, vitamins, and herbal products. Mercaptopurine should not be used with azathioprine unless instructed otherwise. Certain medicines like mesalamine, olsalazine, sulfasalazine, trimethoprim-sulfamethoxazole, or warfarin can affect how Mercaptopurine works. Using Mercaptopurine with allopurinol may require a dose adjustment. It is also important to consult a doctor before getting vaccines.
What are some warnings associated with Mercaptopurine use? Mercaptopurine may cause birth defects if used during conception or pregnancy. Effective birth control should be used during treatment and for a specified period after the last dose. Breastfeeding should be avoided. Patients with certain conditions like kidney disease, liver disease, blood or bone marrow problems, autoimmune disease, or infections should inform their doctor. The medicine may lead to liver problems, increased risk of new cancers, low blood sugar in children, bleeding tendencies, and skin sensitivity to sunlight.
What are some possible side effects of Mercaptopurine? Serious side effects that require immediate medical attention include allergic reactions, gastrointestinal issues, fever, redness or swelling of the skin, joint pain or swelling, abnormal bleeding or weakness, weight loss, and swollen glands. Less severe side effects may include changes in skin color, rash, diarrhea, and hair loss. Any suspected side effects should be reported to the doctor.