
Treatment of Overactive Bladder: 2 Beta-3 AR Agonists
April 13, 2021
First Smart Hospital in Hong Kong
April 18, 2021The following content will be displaying general guidelines for TPN. The information below to be used for education purposes only and not to substitute your clinical judgment.

*General Guidelines for TPN*
Planning nutritional therapy for hospitalized patients.
A) Nutritional screening:
it’s an initial and ongoing process of identifying characteristics known to be associated with nutrition problems in order to identify patients who are nutritionally at risk for malnutrition or are malnourished.
B) Assessment of patients:

- Medical history review:
For past and present recent medical problems that have affected or may affect nutritional status. For example, medications, diagnostic procedures, surgeries, chemotherapy, radiation, etc.
2. Medical record review:
To identify factors that may affect nutritional status.
For example:
- Existing nutrient deficiency (ies).
- Acute or chronic illness with nutritional consequences.
- History of nutritional related problems.
- Medications with potential drug/nutrient interactions.
- Psychosocial factors, such as, alcoholism, smoking, financial situations.
- Nutritional assessment:
- Nutritional history to identify risk of malnutrition.
- Pattern of weight loss (continuing, stabilizing or reversing).
- Physical examination to include Anthropometrics (triceps skin fold mid upper arm circumference) to estimate subcutaneous to estimate fat reserve and muscle.
- Biochemical assessment: which including visceral proteins, (albumin, transferring pr pre-albumin).
- Immunocompetence secondary to malnutrition, (total lymphocyte count).
- Calories requirement assessment to establish nutritional needs for each patient:
- Basal energy expenditure – BEE and total energy expenditure -TEE
- Metabolic status, which is trauma, sepsis or burns.
- Route of administration, such as oral, enteral, peripheral or central IV.
| Age in years | Recommended Caloric Intake |
| 0-1 | 80-140 kcal/kg/day |
| 1-3 | 85-95 kcal/kg/day |
| 4-6 | 80-90 kcal/kg/day |
| 7-10 | 70-80 kcal/kg/day |
| 11-14 | 55-65 kcal/kg/day |
| 15-adults | 25-50 kcal/kg/day |
- Protein requirements assessment:
| Amino Acids requirements | |
| 0-6 months | 2-3 g/kg/day |
| 6m-6 years | 2-2.5 g/kg/day |
| 7-12 years | 1.5-2 g/kg/day |
| > 12 years-adults | 0.8-1.5 g/kg/day |
- Recommended Dietary allowance (RDA) for adults is 0.8 gram per kg of ideal body weight (IBW)
- Disease related requirements (hepatic dysfunction, renal dysfunction, dialysis and non dialysis requirements etc.
- Metabolic stress / trauma requirements range is one to 2.5 grams per kg per day according to severity of condition.
- Non protein calories to nitrogen ratio is needed for optimal protein synthesis.
- The ratios of a standard nutritional formulas to achieve positive nitrogen balance are typically about 100 to 150 non protein calories per gram of nitrogen. Lower ratios are indicated for stress or trauma, while higher ratios for pediatrics, non-stress patients or for those with impaired protein metabolism.
- Nitrogen balance is used to determine the amount of nitrogen required to maintain nitrogen equilibrium
- Protein should be only used to build new tissue and not to contribute in daily calorie can intake (glucose and lipid should be used in sufficient quantities to avoid protein catabolism)
C) Prescribing of TPN:

1. Fluid requirements:
Any fluid imbalance should be corrected; fluid intake urine output and IV drugs will be taken into account when circulating or calculating fluid requirements.
The TPN fluid should:
- Contain the required total calories.
- Provide sufficient hydration and prevent hyper-osmolarity problems.
- Replace the insensible losses that occur during surgery, for pyrexial or hyperventilating patients.
Fluid restrictions is for the deciding factor in selecting hypertonic concentrated solutions for infusion through central vein rather than a more diluted solution for peripheral administration.
Maintenance requirements calculated as following:
Neonates: 80-150ml/kg/day according to gestational age, post natal age, incubator condition and phototherapy.
The following table shows the fluid volume in ml/kg/day for the given age of the newborn up to one month, and that volume will be corresponding to the infant weight.
| Day 1 | Day 2 | Day 3 to 1 month | |
|---|---|---|---|
| wt< 1200 gm | 80-100 | 100-120 | 120-140 |
| 1201 – 2500 gm | 70 | 80-100 | 100-120 |
| 2501 – 4500 gm | 50-60 | 60-80 | 100 |
Infants to adults:
| Wt. (1-10 kg) | 100ml/kg/day |
| 10.1 – 20 kg | 1000ml + 50ml/kg above 10 kg |
| >20 kg | 1500ml + 20ml/kg above 20 kg |

2. Protein as amino acid solutions:
- 1gm protein yields 4kcal of energy.
- 1gm nitrogen contains 6.25 gm protein.
- Aminoplasmal 10%(500ml / bottle) is the available regular amino acid solution.
- Specialized amino acids formulas will be available if efficacy has been approved:
- For uremic patients.
- For patient with liver insufficiency (hepatic encephalopathy).
- For neonates, infants and young children: Primene 10%.
The increase in concentration should be gradual, till maximum recommended strength:
| Age | Start at conc. of | Increased by |
|---|---|---|
| Neonates | 0.5% amino acid solution | 0.5% every other day |
| Infants | 1% amino acid solution | 0.5% every day |
| Children | 1% amino acid solution | 0.5% every day |
| Adults | 4.25% amino acid solution |
Osmolarity of TPN solution: The maximum osmolarity must not exceed the following values when administered peripherally:
| Age group | Peripheral line TPN |
|---|---|
| Neonates and infants | 1100 mOsmol/L |
| Pediatric < 11 years | 1050 mOsmol/L |
| Adolescent – Adult | 900 mOsmol/L |
3. Dextrose:
| IBW | Maximum utilization of glucose | Maximum rate of oxidation |
|---|---|---|
| < 8 kg | 25 gm/kg/day | 17 mg/kg/min |
| 8 – 15 kg | 20 gm/kg/day | 17 – 14 mg/kg/min |
| 15.1 – 25 kg | 16 gm/kg/day | 14 – 11 mg/kg/min |
| 25.1 – 50 kg | 10 gm/kg/day | 11 – 7 mg/kg/min |
| > 50 kg and adults | 8 gm/kg/day | 5 mg/kg/min |
Begin TPN dextrose infusion at the same dextrose load provided by the current IV fluids, advance 1-3 mg/kg/min as tolerated, till maximum oxidation rate.
The rate of dextrose infusion should be limited to its maximum rate of oxidation, to avoid excess glucose that will be diverted to non oxidative pathway (glycogen storage, hepatic lipogenesis, cholestasis, hepatomegaly, etc.).
- 1 gm Dextrose provides 3.4 kcal of energy.
- It is supplied as 25%, 50%, or 70%.
- Maximum allowable concentrations are 12.5% when given by peripheral vein, and 20-25% when given by central vein, concentrations higher than 25% may be indicated for fluid restricted patients.
- Infusion and oxidation of high amount of glucose will require a compensatory increase of minute ventilation due to increased CO2 production.
- The increase in concentration should be gradual, till maximum recommended strength to allow appropriate response of endogenous insulin and to avoid osmotic diuresis:
| Age | |||
|---|---|---|---|
| Premature and newborn infants | 5% initially | Increased by 2.5% every 2 days | Maximum 10% if peripheral line and to 20% if central line |
| Older infants and children | 5% initially | Increased by 2.5% every day | Maximum 10% if peripheral line and to 20% if central line |
| Older children and adults | 5% initially | Increased by 5% every day | Maximum 12.5% if peripheral line and to 25% if central line |
Urine sugar spills:
For +1 and +2 no insulin is required.
For +3 obtain stat blood glucose; if exceeds 250 mg%.
Commence blood glucose every 4 hours and potassium measurements and proceed as follow:
| Blood glucose | Insulin IV |
|---|---|
| 250 to 300 mg % | 5 U regular insulin |
| 301 to 350 mg % | 10 U regular insulin |
| 351 to 400 mg % | 15 U regular insulin |
Further management will be determined on basis of response to above.
- insulin should be used cautiously to avoid hypoglycemia and because it promotes the deposition of fatty acids in body fat stores, making them less available for important biochemical pathways.
- Until a patient is stabilized on a consistent dosage of insulin, it is more cost effective to provide insulin separately to avoid wasting of TPN formulations that might be discarded if the insulin dosage needs to be changed.
- 1/2 to 2/3 the previous day’s sliding scale requirements may be added to daily TPN formula.
- Recommended maximum insulin per liter is 50 U although up to 100 U/Liter has been added with satisfactory results.
4. Lipids:
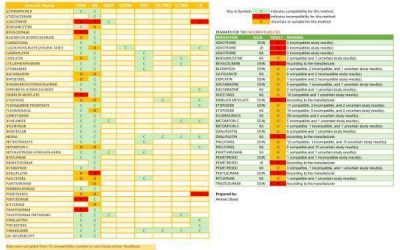
- Lipofundin 20% is available. It contains a mixture of medium and long chain triglycerides (MCT/LCT) in 1:1 ratio.
- 20% emulsion provides 2kcal/ml.
- Fat is concentrated source of calories in an isotonic medium that is useful for peripheral administration.
- It is a source of essential fatty acids (EFA )required the for prevention or treatment of essential fatty acid deficiency that may develop during extensive parenteral nutrition with dextrose.
- It substitutes carbohydrates when dextrose must be limited due to glucose intolerance or excessive respiratory load.
- Infuse lipid over 20 hours to allow plasma lipid free for 4 hours before morning blood sampling as lipid me interfere with lab results as well as inaccurate plasma TG levels.
- Lipid syringes and tubing should be protected from light by wrapping it in foil.
- Daily requirements:
Lipids should not provide more than 60% of the non-protein calories (maximum 3 gm/kg)
| Age | Initially | Increased by | Maximum daily dose |
|---|---|---|---|
| Premature infants | 0.5 gm/kg/day | 0.5-1 gm/kg/day | 3 gm/kg/day |
| Infants | 1 gm/kg/day | 0.5-1 gm/kg/day | 3 gm/kg/day |
| Older children and adults | 1 gm/kg/day | 0.5-1 gm/kg/day | 2 gm/kg/day |
- Infusion rate of lipids:
In pediatric: 0.1 ml/min for the first 10-15 minutes (if no allergic reaction, respiratory distress, or fever occurs, you may continue at a regular rate for the day s dose).
In adults: on the first day of fat emulsion only, run test infusion at 60 ml/hour for 30 minutes and observe the patient for cardiovascular instability, dyspnea, chest pain, CNS, and GI symptoms. If there are no untoward effects, proceed with the remainder of fat emulsion at 80 ml/hour. - The maximum rate of infusion not to exceed 1.5 ml/kg/hour (120 ml/h for the average adult).
- Infusion of lipid can be via peripheral catheter, which must be new and sterile and will be used for fat emulsion only. DO NOT use existing IV lines and DO NOT use the line for any other procedures or infusions.
- Lipid can be given by the same line of dextrose-amino acid solution via a Y-connector proximal to the filter. Y-connector is to be changed daily.
- Don’t interrupt dextrose-amino acid solution to infuse fat emulsion.
- FILTER SHOULD NOT BE USED WITH LIPIDS INFUSION.
- Laboratory slips for T.bilirubin, sodium, potassium, and calcium must be marked (ultracentrifuge) to ensure accurate laboratory values.
- All patients should have triglycerides, cholesterol, and free fatty acids levels determined once weekly. If TG level > or equal to 400 mg % or if FFA/albumin molar ratio is 4:1, the dose must be adjusted.
- In neonates: in presence of jaundice requiring phototherapy, lipid > 2 gm/kg/day should be avoided.
5. Electrolytes:
- Intracellular electrolytes principally potassium, magnesium, and phosphate should be provided for optimum utilization of amino acids.
- Extracellular electrolytes (sodium, calcium, and chloride in sufficient quantities) should be given.
- TPN shouldn’t be used to correct major electrolyte abnormalities, in this regard; electrolytes will be added thru separate IV line and not directly added to TPN bag that is currently infused.
- Phosphate should be added in the first few TPN bags to all patients except if contraindicated.
| Electrolytes | Dosage forms | Concentration | Adult requirements | Pediatric |
|---|---|---|---|---|
| Potassium | Potassium chloride 15% Potassium phosphate Potassium acetate | 2 meq/ml 4.4 meq/ml 2 meq/ml | 70-180 meq/day | 2-3 meq/kg/d |
| Magnesium | Magnesium sulfate 50% | 4 meq/ml | 8-32 meq/day | 0.25-0.5 meq/kg/d |
| Phosphate | Sodium phosphate Potassium phosphate | 3 mmol/ml 3 mmol/ml | 9-30 mmol/day | 0.5-2 mmol/kg/d |
| Sodium | Sodium chloride concentrate Sodium acetate | 4 meq/ml 2.5 meq/ml 2 meq/ml | 60-150 meq/day | 2-4 meq/kg/d |
| Calcium | Calcium gluconate 10% | 4.5 meq/10ml | 5-40 meq/day | 0.5-3 meq/kg/d |
| Chloride | Sodium chloride 23.4% Or Sodium chloride 14.6% | 4 meq/ml 2.5 meq/ml | 60-150 meq/day | 2-4 meq/kg/d |
| Acetate | Sodium acetate Potassium acetate |
6. Vitamins:
- Cernevit is available as intravenous multivitamin combination of both water and fat-soluble vitamins presented in one vial
| Vitamin | Each 5 ml cernevit contains: |
|---|---|
| Vitamin A | 3500 IU |
| Thiamine | 5.80 mg |
| Riboflavin | 5.67 mg |
| Pyriodoxine | 5.50 mg |
| Vitamin B12 | 6 mcg |
| Biotin | 69 mcg |
| Folic acid | 414 mcg |
| Niacinamide | 46 mg |
| Dexapanthenol | 16.15 mg |
| Vitamin C | 125 mg |
| Vitamin E | 10.2 mg |
| Vitamin K1 | _ |
| Vitamin D | 220 IU |
- The usual daily dosage of adults is 10 ml.
- Pediatric daily dosage:
| Wt. (kg) | Dosage (ml) |
|---|---|
| < 1 kg | 1.5 ml |
| 1-3 kg | 3 ml |
| > 3 kg and up to 11 years of age | 5 ml |
- Intramuscularly administered vitamins:
1. Vitamin K1 (phytonadione):
| Infants | 0.25-0.5 mg | Twice weekly |
| Older children | 2 mg if < 2 years 5 mg if 2-5 years 10 mg if > 5 years | Once weekly |
| Adults | 10 mg IM | Weekly to all adult patients, unless the patient is on daily vitamin K |
2. Vitamin B12 (cyanocobolamine):
Infants: 50 mcg twice monthly.
Older children: 100 mcg initially and then monthly.
Adults: May be given additionally once a month (1000 mcg) or weekly as required.
*Folic acid is present in Cernivit.
7. Trace elements:
| Trace element | Infants and toddlers mcg/kg/day | Children mcg/kg/day | Adults |
|---|---|---|---|
| Copper | 20 | 20 | 30 mcg/day |
| Zinc | Premature: 300 < 3 months old: 150 > 3 months old: 100 | 50 | 4 mg/day |
| Manganese | 1 | 1 | 50 mcg/day |
| Chromium | 0.2 | 0.2 | 10-15 mcg/day (20 mcg/day if intestinal loss) |
| Selenium | 2 | 2 | 30 mcg/day |
| Molybdenum | 0.25 | 0.25 | 5 mcg/day |
| Iodide | 1 | 1 | 1 mcg/day |
- Tracutil, a formulation of 9 trace elements including iron is available for use in TPN for adults.
- Pediatric trace elements shall be used for neonatal and pediatric patient.
- Additional supply of zinc and selenium may be needed especially in acute catabolic states, in patients undergoing medium to long-term parenteral nutrition and when there is increased intestinal losses of zinc.
- Caution in case of impaired renal or liver functions.
Heparin:
0.5-1 unit/ml of the TPN solution added, this amount over 24 hours has little or no effect on a PTT.
Albumin:
Maximum in TPN = 60 gm/day or 20 gm/L.
D) Monitoring the patient:
Frequency of routine monitoring should be increased in critically ill patients.
| Routine monitoring parameters | Frequency |
|---|---|
| Urinary glucose, ketones and specific gravity | Every voided specimen until stable, then daily |
| Finger stick glucose | Every 6 hours until stable |
| Temperature, Vital signs | Every 4 hours |
| Weight, intake and output | Daily |
| Serum glucose, Na, K, CL, HCO3, osmolarity, creatinine, and BUN | Daily until stable, then twice weekly |
| Magnesium, Calcium, and Phosphorous | Daily until stable, then once weekly |
| CBC, and prothrombin time, INR | Baseline then weekly |
| Serum protein, albumin, prealbumin | Baseline then weekly |
| LFTs | Baseline then twice weekly |
| Serum cholesterol and triglycerides | Every day for 2 days then weekly |
| Blood ammonia | Baseline then weekly in renal and hepatic pt. |
TPN complications:
- Most of complications can be avoided by proper precautions and close monitoring of the patient.
- NST team leader should be notified immediately.
- IV insertion site shall be checked by the nurse every shift for infection, infiltration, extravasation and phlebitis.
- Dressing and TPN administration (rate, time of solution change) shall be checked by the nurse every shift.
Suspicion of sepsis:
- In the event of sudden pyrexia or suspicion of sepsis, the nurse should stop the TPN and inform the attending physician immediately.
- A full septic screen should be initiated:
1. Catheters tips when removed should always be sent for culture and sensitivity.
2. A specimen of TPN collected for culture and sensitivity.
3. Blood serum sample for culture, sensitivity and electrolytes.
4. Lumbar puncture (CSF for culture, sensitivity, cell count, lytes and glucose).
5. Chest X-ray.
6. Urine for culture and sensitivity.
7. Endotracheal aspirate (if intubated) for culture and sensitivity.
8. Peripheral swabs if indicated.
Metabolic complications:
Awareness of the patient problems and the predisposing factors will facilitate their prevention
| Problem | Predisposing factors | Management |
|---|---|---|
| Hyperglycemia | 1-Sepsis 2-Deficit of potassium or phosphorous 3-Insufficient insulin 4-Medications e.g. corticosteroids | 1-Sepsis workup and treatment 2-Increase potassium or phosphorous provision 3-Titrate insulin 4-Reduce rate of glucose infusion |
| Hypoglycemia | 1-Abrupt withdrawal or interruption of TPN infusion 2-Anabolism 3-Excess insulin | 1-Begin dextrose 50% infusion -Ensure correct tapering of TPN infusion -If accidental disconnection; start dextrose 10% infusion at the same rate of TPN infusion 2-Monitor blood glucose and potassium 3-Decrease insulin |
| Problem | Predisposing factors | Management |
|---|---|---|
| Hypokalemia | Large glucose infusion Excessive GI losses (drains, fistula, diarrhea, ..) Excessive urinary losses (diuretics, amphotericin, ..) Potassium deficit | Potassium supplements |
| Hypophosphatemia | Phosphate binding antacids Anabolism Diabetic ketoacidosis Phosphate free dialysis | Discontinue phosphate binder Increase phosphate intake Feeding gradually |
| Hypomagnesemia | Insufficient intake Chronic diarrhea Extensive small bowel resection | Increase magnesium intake |
| Hypocalcaemia | Insufficient intake Malabsorption Diuretics Insufficient vitamin D intake Hypothyroidism Mg deficiency | Calcium replacement Magnesium replacement |
| Hyponatremia | Relative excess of water Insufficient intake Pyrexia Sweating GI losses | Increase sodium provision |
| Metabolic acidosis | High output GI fistula Excess amino acids Excess chloride Renal failure | Decrease chloride or increase acetate provision Decrease amino acids in TPN |
| Azotemia | Dehydration Impaired renal function Excess nitrogen infusion | Correct dehydration Increase E:N ratio |
| Elevated LFTs | Excess dextrose Extended enteral feeding Stress Infection EFA deficiency Excessive nutrients | Provide lipid, decrease Dextrose, or use cycling TPN |
| Hypertriglyceridemia | Impaired clearance | Hold IV lipid if ser.TG> 400 mg% (4.5 mmol/L) |
| Osmotic diuresis | Failure to recognize initial hyperglycemia and increased glucose in urine | Reduce infusion rate Insulin to correct hyperglycemia |
| EFA difficiency | Insufficient provision of fat | Provide lipid |
| Excess CO2 production (PCO2) | Excess dextrose intake | Decrease dextrose and increase fat intake if possible, increase ventilation |
Complications related to catheter insertion:
Pneumothorax, puncture of subclavian or carotid artery and air embolism.
Septicemia related to the catheter:
(Vancomycin is the drug of choice), fever should be investigated on occurrence and TPN lines should be changed if no other cause is found, catheter tips must be cultured if the patient becomes septic;
- If the culture result is positive; the replacement catheter will be removed and a new one will be inserted in different site.
- If the culture result is negative; the replacement catheter will not be removed.
E) Termination of TPN:
- Ensure TPN infusion is never stopped abruptly unless absolutely necessary.
- Check blood sugar levels after TPN is being discontinued until stability assured; blood glucose should be checked every 15-60 min after TPN discontinue.
- In the event of disconnection, TPN may be stored in the fridge. However aseptic technique must be utilized and the integrity of the TPN maintained to prevent sepsis and unstable blood sugar. If aseptic integrity is compromised a new preparation of TPN will be required.
- Enteral nutrition (EN) may be used in the transitional phase between parenteral nutrition (PN) and normal oral intake; gradual reduction of PN over a few days, while EN gradually instituted and increased over the same period of time in a way that total intake remains constant.
Temporary discontinuation of TPN for surgery or investigation:
- Taper TPN by reducing the infusion rate as ordered by the attending physician (20 ml every 15 min until the flow rate is zero).
- Heparin lock the catheter line when TPN administration is discontinued for more than 2 hours using a dilution of 500 u of heparin in 500 ml of normal saline (Heparin should be infused at a rate less than 2 ml/hour).
Accidental disconnection of TPN:
- Commence 10% dextrose infusion immediately for 4-6 hours including while lines are changed., run at the same rate as the TPN was infusing via a different port of access to avoid complications of sepsis of TPN line.
- The TPN catheter tip, blood sample and a sample of the TPN should be sent to microbiology for culture and sensitivity testing whenever the line is removed even in the event of the patient’s death.
Cycling TPN:
It is a maneuver to further reduce the pathophysiologic consequences of TPN administration. It needs to be achieved gradually and the usual goal is to infuse the necessary volume of TPN and lipid over a 16-18 hours period. One hour at each end of the infusion time will have the solution running at half the normal rate to allow the pancreas to adjust insulin/glucagon secretion to prevent hypo-or hyperglycemia. To calculate these rates divide the total volume of TPN/day by the number of hours for infusing minus one to obtain the rate of infusion during the main period of infusion. One half that rate is the step-up and step-down rate. Running D10% solution or other fluid should be unnecessary if the patient has been gradually tapered to this regimen from a 24-hour infusion protocol. Infuse other IV fluids over the remaining 6-8 hours or TKO with the TPN fluid (10 ml/hour).
References:
- Koda K, APPLIED THERAPEUTICS THE CLINICAL USE OF DRUGS; 10th edition 2002.
- R. Walker, C. Edwards; Clinical pharmacy and therapeutics; 3rd edition 2003.
- University of Arizona medical center; guidelines for TPN in adults.
- V. Horn; pediatric parenteral nutrition; hospital pharmacist; VOL. 10 February 2003.
- Royal Prince Alfred hospital; Department of Neonatal Medicine Protocol Book; Total Parenteral Nutrition; Sept. 1999.
- Samuel C., Karen C., etal; Nutrition Management in the ICU; CHEST 1999; 115:145S-148S.
- University of California; Intensive Care Nursery House Staff Manual; Neonatal Parenteral Nutrition. 2004.











5 Comments
Excellent Informative & fruitful General Guidelines for TPN Please note that ASPEN & ESPEN in Facts against Myths Use PN instead of TPN as the latter becomes an Old term.
Could you please advise me about the Method of analysis? & sampling Methods of the Parenteral Nutrition with great thanks
Kindest Regards
Emhemmed Khsheba MOH Libya.
Thanks for your comment, here is the info you requested, kindly tell me if it’s outdated according to your latest research:
Method of Analysis
Macro-Nutrient Analysis: This involves the determination of the concentrations of nutrients such as proteins, carbohydrates, and lipids in the parenteral nutrition solution.
Protein: Biuret method or Kjeldahl method can be used for protein estimation.
Carbohydrates: The Phenol-Sulfuric Acid method is often used for carbohydrate estimation.
Lipids: The Vanillin Phosphoric Acid method or colorimetric assays can be used for lipid estimation.
Micro-Nutrient Analysis: This refers to the determination of vitamins, trace elements, and electrolytes in the solution.
Vitamins: High-performance liquid chromatography (HPLC) can be used to analyze vitamins.
Trace Elements: Atomic absorption spectroscopy or inductively coupled plasma mass spectrometry can be used for trace elements.
Electrolytes: Ion-selective electrodes can be used to measure electrolytes.
Sterility Testing: This is crucial to ensure that the parenteral nutrition solution is free from bacteria, fungi, and endotoxins.
Bacterial and fungal testing: This is done by inoculating a portion of the solution onto various agar plates or into broths and incubating for a specific period.
Endotoxin testing: This is done using Limulus Amoebocyte Lysate (LAL) test.
Sampling Methods
Random Sampling: A particular batch of parenteral nutrition solutions is selected at random for testing. This provides an overview of the quality of the entire batch.
Systematic Sampling: Samples are taken at regular intervals throughout the manufacturing process. This helps to identify at which point, if any, contamination or errors may occur.
Acceptance Sampling: Samples are taken from each batch and tested. If the sample passes the tests, the entire batch is accepted.
Quarantine Sampling: This involves isolating a batch of solutions until they have been tested and confirmed to meet all necessary standards.
Thank you very much for your fruitful comment, including methods for analyzing parenteral nutrition. If possible, please include the references on which these methods are based.
Awaiting your reply.
best regards.
Emhemmed Khsheba Libya
Regarding your request, please let me know if the information you provided is outdated according to my latest research: –
On a personal level, I cannot say that, what I can only say is useful, productive, and informative. As for the latest I have seen in this regard, the following: –
USP Pharmaceutical Compounding — Sterile Preparations. Official as 01-May 2020.
European Pharmacopoeia 11.0 Parenteral preparations. 07-2021
Thank you so much you informing me about Endotoxin testing: This is done using the Limulus Amoebocyte Lysate (LAL) test. Which is an official test still used in this regard.
But The future of sustainable LAL testing has arrived with ACCs Pyro Smart NextGen recombinant LAL reagent. The new testing technology that delivers the best of traditional methods, combined with the benefits of sustainable recombinant cascade reagents (rCR) The future of LAL testing is bright.
Thank you very much once again for your cooperation and for providing valuable information, and I hope that you will also send me more official Pharmacoepial methods used in the analysis of parenteral nutrition.
Kindest regards
Emhemmed Khsheba Senior & Consultant Pharmacist MSO/MOH Libya
Have a nice weekend all.
Emhemmed Khsheba Libya.