
Sleep apnea is a common sleep disorder that causes interruptions in breathing during sleep. There are two main types of sleep apnea: obstructive sleep apnea, which occurs when the throat muscles relax, and central sleep apnea, which happens when the brain fails to send proper signals to the muscles that control breathing. People with sleep apnea often experience symptoms such as loud snoring, daytime fatigue, and high blood pressure.
Obstructive sleep apnea (OSA) is a common disorder that affects nearly 1 billion adults worldwide, yet over 80% of cases go undiagnosed. This serious sleep disorder causes breathing to repeatedly start and stop throughout the night, preventing restorative sleep. When left untreated, OSA raises risks for numerous health issues like high blood pressure, heart disease, stroke, and type 2 diabetes. Thankfully, a variety of effective treatment options exist today to help individuals manage symptoms and reduce these associated health dangers.
Understanding Sleep Apnea: Symptoms, Causes, and Treatments
Sleep Apnea Overview
Obstructive sleep apnea occurs when throat and airway muscles intermittently relax and collapse during sleep, blocking normal breathing. These episodes can last 10 to 30 seconds each before the brain triggers a brief awakening, allowing breathing to restart. This pattern repeats itself 5 to 30 or more times per hour all through the night for those with OSA.

Sleep apnea is a condition characterized by pauses in breathing or shallow breaths during sleep. It is a serious sleep disorder that can significantly impact an individual’s quality of life. Sleep apnea can lead to various health issues, including an increased risk of heart disease, stroke, and diabetes. If left untreated, it can also result in accidents due to daytime sleepiness and impaired cognitive function.
Definition and Types of Sleep Apnea
Obstructive sleep apnea is the most common type of sleep apnea and occurs when the throat muscles relax, causing the airway to become blocked. Central sleep apnea, on the other hand, happens when the brain fails to signal the muscles responsible for breathing. Both types can have serious consequences if not properly diagnosed and treated.
Prevalence and Risk Factors
Sleep apnea is a prevalent condition, especially among adults. Certain risk factors, such as being overweight, having a large neck circumference, or having a family history of sleep apnea, can increase the likelihood of developing the disorder. It is essential for individuals with risk factors to undergo a sleep study to diagnose sleep apnea accurately.
Diagnosis of Sleep Apnea

When it comes to diagnosing sleep apnea, it is essential to be aware of the signs and indicators that may point towards this sleep disorder. People with sleep apnea often exhibit symptoms such as loud snoring, frequent pauses in breathing during sleep, excessive daytime fatigue, morning headaches, irritability, and difficulty concentrating. These signs can significantly impact an individual’s quality of life and overall well-being.
Signs and Indicators of Sleep Apnea – The most common signs and symptoms of obstructive sleep apnea include:
- Chronic loud snoring
- Gasping or choking during sleep
- Extreme daytime fatigue and sleepiness
- Morning headaches
- Difficulty concentrating
- Irritability
Common signs and indicators of sleep apnea include loud and persistent snoring, gasping or choking sounds during sleep, episodes of breathing cessation witnessed by a bed partner, excessive daytime sleepiness even after a full night’s rest, morning headaches, dry mouth or sore throat upon waking, and irritability or mood swings. It is crucial to recognize these symptoms and seek medical evaluation to determine the presence of sleep apnea and its severity.
Sleep Apnea Drops in Oxygen
Over time, the frequent drops in oxygen from repeated breathing stoppages cause cellular damage due to oxygen deprivation throughout the body. This stresses the cardiovascular system and contributes to many associated health risks like heart attack, congestive heart failure, arrhythmias, stroke, and high blood pressure. The lack of restorative sleep also dampens immunity, cognitive function, mood and emotional health.
How Doctors Diagnose Sleep Apnea
Diagnosing sleep apnea involves a comprehensive evaluation by a sleep specialist or healthcare provider. Medical history assessment and physical examination are typically the initial steps in the diagnostic process. Doctors may inquire about the patient’s sleep patterns, daytime symptoms, and risk factors for sleep apnea.
Additionally, various diagnostic tools and tests, such as overnight polysomnography (sleep study), home sleep apnea testing, and continuous positive airway pressure (CPAP) titration, may be utilized to confirm the diagnosis and determine the most appropriate treatment.
Testing and Screening Procedures
For individuals suspected of having sleep apnea, diagnostic testing is vital to assess the severity of the condition and ascertain the most effective treatment. Polysomnography, considered the gold standard for diagnosing sleep apnea, involves monitoring various physiological parameters during sleep, including breathing patterns, oxygen levels, heart rate, and brain activity. Home sleep apnea testing may also be conducted in certain cases to provide a more convenient and cost-effective diagnostic option. These testing procedures help healthcare providers tailor a personalized treatment plan to manage and alleviate the symptoms of sleep apnea effectively.
Treatment Methods

When it comes to managing sleep apnea, various treatment methods are available to improve breathing patterns during sleep and alleviate associated symptoms. The choice of treatment often depends on the type and severity of the condition, as well as individual preferences and underlying health factors.
CPAP Therapy for Sleep Apnea
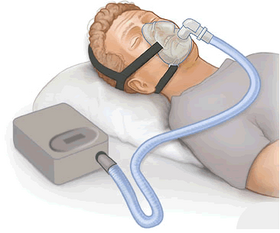
Continuous positive airway pressure (CPAP) therapy is a common and highly effective treatment for obstructive sleep apnea. It involves wearing a CPAP machine that delivers a constant stream of air pressure, preventing the airway from collapsing during sleep. This continuous flow of air helps keep the airway open, allowing for uninterrupted breathing and reducing snoring and apnea episodes.
CPAP devices work by delivering a constant gentle stream of pressurized air through a mask worn over the nose and/or mouth while sleeping. This pressurized air acts as a splint, keeping upper airway tissues open so that breathing is not obstructed throughout the night.
CPAP Therapy in Literature
The effectiveness of CPAP (Continuous Positive Airway Pressure) therapy for treating obstructive sleep apnea (OSA) has been extensively studied and supported by multiple research papers.
Reduction in Drops in Oxygen Levels
The use of CPAP therapy has been shown to effectively reduce drops in oxygen levels during sleep. A study published in the American Journal of Respiratory and Critical Care Medicine found that CPAP significantly reduced the number of desaturation events during sleep in patients with OSA [ijcemand semantic].
Restoring Healthy Sleep Architecture
CPAP therapy has been demonstrated to improve sleep architecture by reducing the number of arousals and awakenings during the night, as well as increasing the amount of time spent in deeper, restorative sleep stages. A study in the journal Sleep Medicine demonstrated that CPAP use led to improvements in sleep architecture, including increased REM sleep and decreased wake time after sleep onset [ijcemand semantic].
Easing OSA Symptoms
Research published in the journal Chest has shown that CPAP use leads to significant reductions in daytime sleepiness and improvements in quality of life for individuals with OSA [ and semantic].
Lowering Associated Health Risks
Long-term and consistent use of CPAP has been associated with a range of health benefits for individuals with OSA. Studies have demonstrated that CPAP use is linked to reductions in blood pressure, arterial plaque, insulin resistance, and stroke risk.
For example, a meta-analysis published in the journal Sleep Medicine Reviews found that CPAP therapy was associated with significant reductions in both systolic and diastolic blood pressure in individuals with OSA [ and semantic].
Improved Sleep Quality and Daytime Functioning
Patients using CPAP therapy as prescribed often report better sleep quality, improved concentration, reduced daytime fatigue, and improved mood. A study in the journal Sleep found that CPAP use led to improvements in subjective sleep quality, as well as reductions in daytime sleepiness and fatigue [ and semantic].
CPAP Challenges
However, some patients struggle to acclimate to wearing CPAP equipment for lengthy nightly usage due to mask discomfort, nasal dryness or claustrophobia.
Thankfully, today’s CPAP equipment offers a wide range of personalized mask types and air pressure settings to increase comfort and compliance rates. Adding heated humidification, trying different mask styles (nasal, full-face, nasal pillows) and slowly adjusting duration of use can also boost tolerance for chronic CPAP therapy.
Other Treatment Options

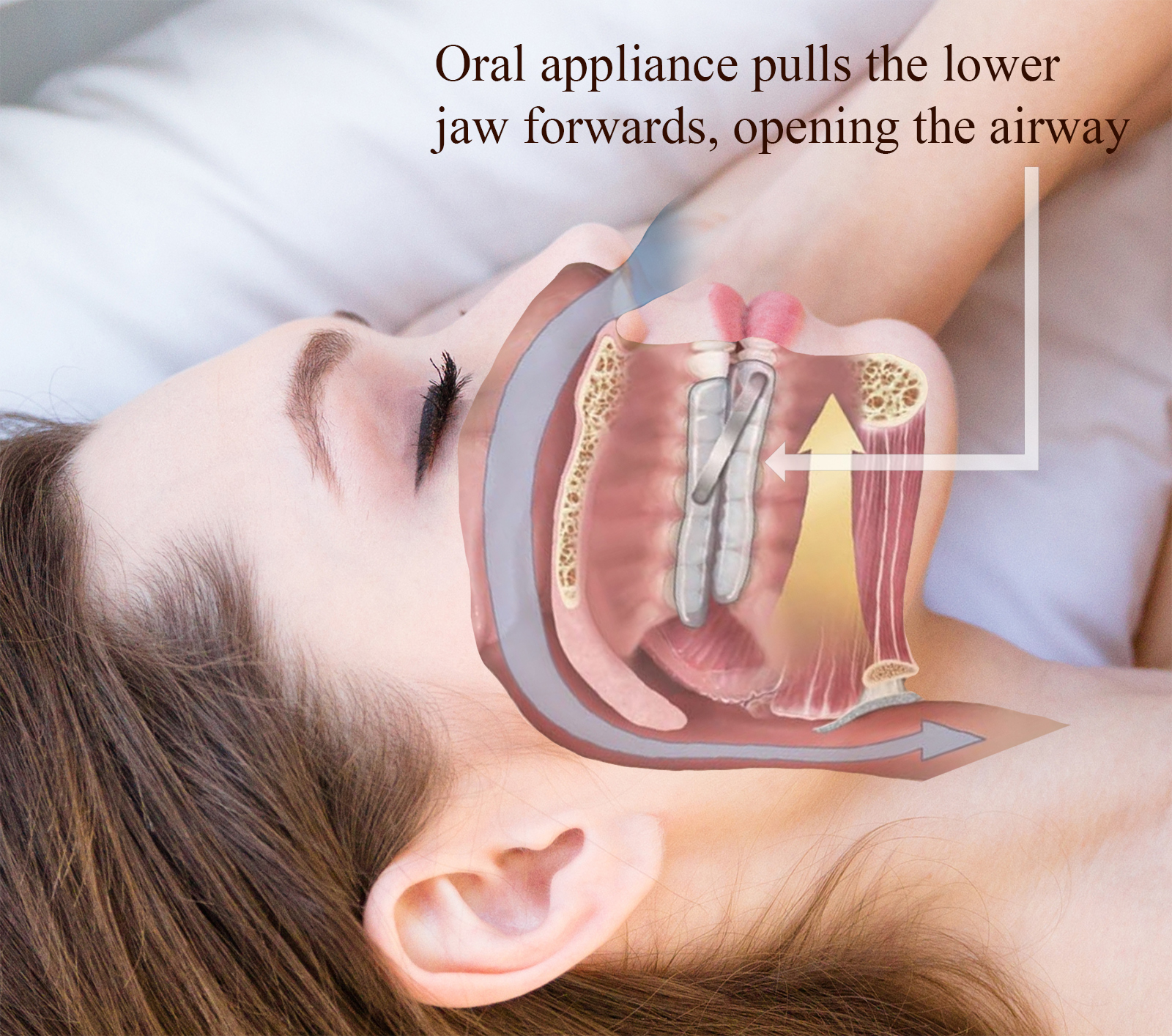
Aside from CPAP therapy, alternative treatments for sleep apnea may include oral appliances that help keep the airway open, lifestyle modifications such as weight loss and positional therapy, and surgery in some cases where other treatments have not been effective.
Custom-made oral sleep apnea appliances are another first-line treatment approach today, especially for those with mild to moderate OSA. Oral appliances look similar to orthodontic devices or sports mouth guards, fitting snugly over the teeth.
By supporting the jaw in a forward projected position, oral appliances help maintain an open, unobstructed airway all through the night.
Oral Appliances Therapy in Literature
The clinical evidence from various research papers supports the effectiveness of oral appliance therapy (OAT) in reducing obstructive sleep apnea (OSA) symptoms and improving sleep-related parameters for many patients.
Effectiveness of Oral Appliance Therapy (OAT)
- Improvement in Polysomnography Parameters: Research has shown that OAT can effectively improve polysomnography parameters, including the apnea-hypopnea index (AHI) and oxygen desaturation levels during sleep. Studies have demonstrated significant reductions in AHI and improvements in oxygen saturation levels with the use of oral appliances [Semantic] [ and Semantic] [ and Semantic] .
-
Predictive Value of Screening Instruments: Questionnaires such as the Berlin Questionnaire (BQ) and Epworth Sleepiness Scale (ESS) have been found to be predictive of improvements detected by sleep studies during biomimetic oral appliance therapy (BOAT) use. These screening instruments may provide valuable insights into the potential outcomes of OAT for individuals with OSA [Semantic] .
- Patient Adherence and Satisfaction: Oral appliance therapy has been associated with greater patient adherence and satisfaction compared to other treatment modalities such as continuous positive airway pressure (CPAP). Patients often report ease of portability for travel, reduced equipment, and quiet operation for bed partners as key benefits of oral appliances [Sleepmedres and Semantic] [ and Semantic] [IGMpublication and Semantic] .
- Effectiveness in Moderate to Severe OSA: Studies have demonstrated the effectiveness of oral appliances in patients with moderate or severe OSA, with significant reductions in AHI and improvements in sleep architecture. The use of mandibular advancement devices has been shown to be effective in improving AHI and symptoms in a majority of subjects from various studies [Semantic] [ and Semantic] [ and Semantic] .
- Multifactorial Nature of Response: The response to mandibular advancement device (MAD) therapy has been found to be multifactorial, with factors such as age and deep bite influencing the reduction in AHI. This indicates that the response to MAD therapy may vary based on individual patient characteristics [ and Semantic] .
Considerations for Oral Appliance Therapy
- Customization and Follow-Up Adjustments: Customization and follow-up adjustments are critical to achieving an optimal fit and symptom relief from oral appliances. Devices tailored to the individual patient’s dentition and capable of manipulating the degree of mandible advancement are essential for maximizing the benefits of OAT [Sleepmedres and Semantic] .
- Adverse Effects and Treatment Compliance: Patients should be informed about potential adverse effects on mastication and the mandibular joint, as these effects can negatively influence treatment compliance. While most adverse effects are minor and transient, patient education and monitoring are important aspects of OAT management [Sleepmedres and Semantic] .
- Long-Term Efficacy and Adherence: Long-term efficacy and adherence to oral appliance therapy are important considerations. Studies have highlighted the need for follow-up supervision to monitor efficacy and adherence over time, with recommendations for device replacement if necessary [ and Semantic] .
Surgical Interventions for Severe Cases
For individuals with severe obstructive sleep apnea or specific anatomical issues contributing to the condition, surgical interventions may be considered.
Surgical options aim to remove or reposition tissues blocking the airway, such as uvulopalatopharyngoplasty (UPPP), maxillomandibular advancement, hypoglossal nerve stimulation (HNS), and less invasive office-based treatments or tracheostomy in extreme cases.
Uvulopalatopharyngoplasty (UPPP)
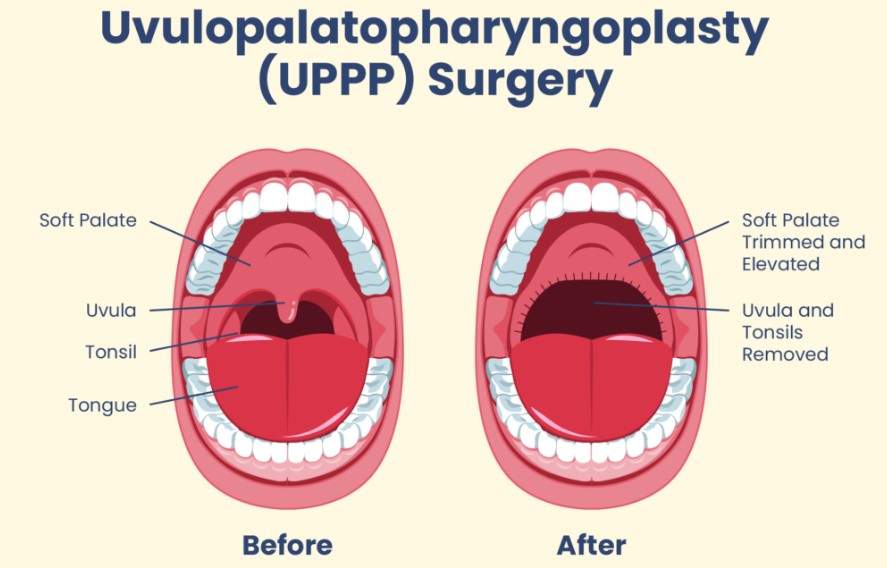
- Incidence and Complications: A study in Taiwan found that the incidence of multilevel UPPP increased from 2000 to 2012, and these surgeries appeared to be associated with a higher risk of complications, particularly readmissions for any reason and bleeding-related readmissions [ and Semantic].
- Long-term Efficacy: Despite the surgical efficacy decreasing over time, UPPP and its modification are an effective surgical method for adult OSA in both the short term and the long term after the surgery [ and Semantic] .
- Predictors of Success: Friedman stage I is a strong predictor for success after UPPP, while Friedman stage III and low hyoid position are negative predictors. Age, body mass index, preoperative apnea-hypopnea index, and other cephalometric measurements were not significant predictors [] and Semantic] .
Maxillomandibular Advancement (MMA)
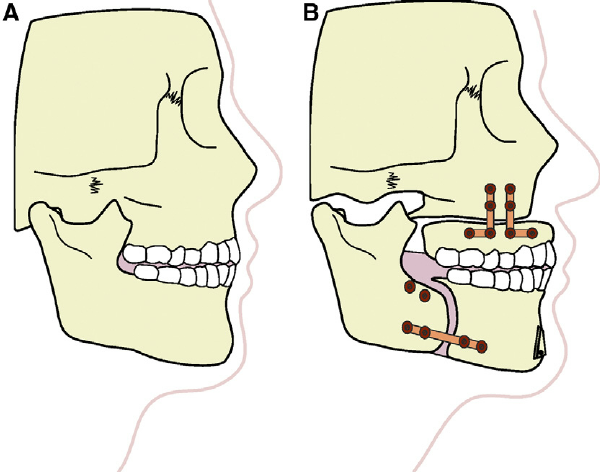
- Long-term Results: MMA is considered the most effective surgical treatment for the management of OSA in adult patients who are not responders to medical treatment. It has been shown to significantly improve respiratory function and facial esthetics [] and Semantic] .
- Subjective Efficiency Evaluation: A study confirmed that MMA surgery in OSA patients improves outcomes, both objectively and subjectively, with the exception of postoperative mandibular function [Semantic] .
- Airway Changes Prediction: Simulation approaches using computational fluid dynamics have been developed to predict maxillomandibular advancement-induced airway changes, facilitating preoperative prediction of the postoperative structural outcome [Semantic] .
Hypoglossal Nerve Stimulation (HNS)
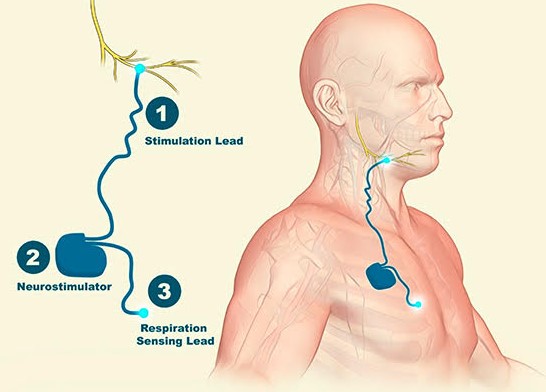
- Efficacy and Patient Satisfaction: HNS has been shown to be an effective treatment for OSA in patients with CPAP intolerance, with the vast majority of patients reporting satisfaction with post-surgical facial aesthetics. It substantially contributes to enhancement of overall quality of life and perceived aesthetic appeal [Semantic] .
- Upper Airway Control: Pilot studies have confirmed that hypoglossal nerve stimulation can prevent pharyngeal collapse without arousing patients from sleep, suggesting that a substantial segment of the patient population with obstructive sleep apnea can be treated with this novel approach [physiology.org and Semantic] .
Special Considerations

When it comes to sleep apnea in children, it is essential to recognize that this condition can affect individuals of all ages, including infants, toddlers, and adolescents. While the symptoms in children may differ from those in adults, common indicators of pediatric sleep apnea include loud snoring, bedwetting, restless sleep, and behavioral issues.
Untreated sleep apnea in children can lead to developmental delays, poor academic performance, and even cardiovascular problems in severe cases. Therefore, early detection and intervention are crucial to ensure the well-being and healthy development of children with sleep apnea.
Effects of Untreated Sleep Apnea
Untreated sleep apnea can have detrimental effects on both physical and mental health. Chronic sleep deprivation caused by untreated sleep apnea can contribute to an increased risk of hypertension, heart disease, stroke, and type 2 diabetes.
Moreover, the cognitive effects of sleep apnea, such as impaired memory, concentration difficulties, and mood disturbances, can significantly impact an individual’s quality of life and overall well-being. It is essential to address and treat sleep apnea promptly to prevent these severe health consequences.
Lifestyle Changes to Improve Sleep Quality
Adopting healthy lifestyle habits can play a significant role in improving sleep quality and managing sleep apnea. Maintaining a regular sleep schedule, practicing good sleep hygiene, such as creating a conducive sleep environment and avoiding stimulants before bedtime, and engaging in regular exercise can positively impact sleep patterns.
Weight management through a balanced diet and physical activity is also crucial, as excess weight can exacerbate sleep apnea symptoms. By incorporating these lifestyle changes, individuals with sleep apnea can improve their overall sleep quality and reduce the severity of their symptoms.
Positional Therapy for Obstructive Sleep Apnea
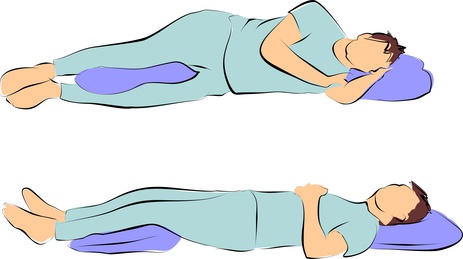
Positional therapy techniques are also simple yet effective OSA remedies to try at home. Since sleep position impacts airway size, avoiding back sleeping prevents the tongue from collapsing backwards and blocking airflow.
To maintain side sleeping all night, wedge pillows and sleep shirts with pockets to hold tennis balls can help minimize tossing and turning onto the back through gentle feedback. Raising the head of the bed by 4 to 6 inches also utilizes gravity to keep passages open. While not universally effective as standalone apnea solutions, excellent research substantiates positional therapy and elevation as useful home remedies improving oxygen levels and easing symptoms for better rest.
Positional Therapy in Literature
- “Positional Therapy for Obstructive Sleep Apnea: Therapeutic Modalities and Clinical Effects” by Ki-Il Lee, J. Choi, published in Sleep Medicine Research in 2023, provides insights into the promise of positional therapy in improving apneic events and lowest oxygen saturation in patients with position-dependent sleep apnea. The paper also compares positional therapy to positive airway pressure treatment and reports its non-inferior effects, while achieving better compliance. Source
- “Combination of positional therapy with positive airway pressure for titration in patients with difficult to treat obstructive sleep apnea” by A. Goyal et al., published in Sleep and Breathing in 2021, explores the combination of positional therapy with positive airway pressure for titration in patients with challenging obstructive sleep apnea. Source
- “The predictive value of drug-induced sleep endoscopy for treatment success with a mandibular advancement device or positional therapy for patients with obstructive sleep apnea” by P. Bosschieter et al., published in Sleep and Breathing in 2021, investigates the predictive value of drug-induced sleep endoscopy for treatment success with mandibular advancement device or positional therapy for obstructive sleep apnea patients. Source
- “Effect of positional therapy on the sleep apnea-specific hypoxic burden and pulse rate response in children with positional Obstructive Sleep Apnea” by L. Xiao et al., published in Sleep Medicine in 2024, focuses on the effect of positional therapy on the sleep apnea-specific hypoxic burden and pulse rate response in children with positional obstructive sleep apnea. Source
- “Efficacy of Positional Therapy Prototype for Patients with Positional Obstructive Sleep Apnea” by S. Lokavee et al., presented at the 2020 12th International Conference on Knowledge and Smart Technology (KST), discusses the efficacy of a positional therapy prototype for patients with positional obstructive sleep apnea. Source
Sleep Apnea Combination Therapy
- Rather than any standalone apnea solution, research increasingly highlights utilizing combined treatment modalities for superior obstructive sleep apnea improvement. This synergistic approach merges the mechanism of action from distinct therapies like PAP technology plus custom oral appliances and/or anti-reflux medication if warranted. Source
- additional research also indicates supplemental oxygen concentrators help further boost blood oxygen saturation. Source

FAQs
Q: What are the symptoms of sleep apnea?
A: Symptoms of sleep apnea include loud snoring, gasping for air during sleep, morning headaches, excessive daytime sleepiness, and difficulty concentrating.
Q: What are the causes of sleep apnea?
A: Sleep apnea happens when the muscles in the back of your throat relax too much to allow normal breathing, leading to upper airway collapse or blockage during sleep.
Q: How is sleep apnea treated?
A: Treatment for sleep apnea may include lifestyle changes, such as weight loss or sleeping on your side, continuous positive airway pressure (CPAP) therapy, oral appliances (mouthpiece) to keep the airway open, or surgery in severe cases.
Q: Can children have sleep apnea?
A: Yes, sleep apnea can occur in children, especially those with enlarged tonsils or adenoids, obesity, or craniofacial abnormalities.
Q: What are the risk factors for sleep apnea?
A: The risk for sleep apnea increases with factors such as obesity, older age, family history of sleep apnea, smoking, and certain anatomical features like a thick neck or small upper airway.
Q: How is obstructive sleep apnea different from central sleep apnea?
A: Obstructive sleep apnea happens when the airway is blocked, usually by the soft tissues in the back of the throat, while central sleep apnea happens when the brain fails to send signals to the muscles that control breathing.
Q: What are the treatments for obstructive sleep apnea and central sleep apnea?
A: Treatments for obstructive sleep apnea may include CPAP therapy, oral appliances, or surgery, while central sleep apnea may require treatment with servo-ventilation or adaptive servo-ventilation.













